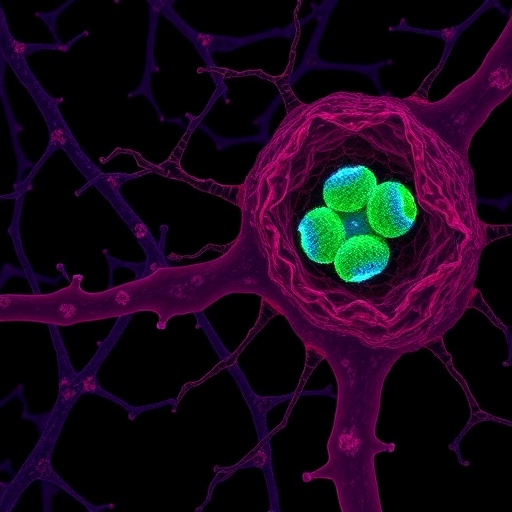
In a groundbreaking study set to redefine therapeutic strategies for type 2 diabetes mellitus (T2DM), researchers have unveiled a novel approach that targets pancreatic β cell autoinflammation through precise mitochondrial intervention. The innovative work, published in Nature Communications, introduces islet-mitochondrial sequential targeting nanomedicines to inhibit Uncoupling Protein 2 (UCP2), a pivotal player in the metabolic dysfunction and inflammatory processes underlying β cell deterioration in T2DM. This advancement not only deepens our understanding of the intricate interplay between mitochondrial health and β cell function but also opens new avenues for combating the progressive nature of diabetes with unprecedented precision.
Type 2 diabetes is characterized by chronic insulin resistance and the progressive failure of pancreatic β cells, which secrete insulin to regulate blood glucose levels. Central to this deterioration is an often-overlooked contributor: autoinflammation within β cells driven by mitochondrial dysfunction. Mitochondria, the powerhouses of the cell, play a crucial role in energy metabolism, and their compromised function triggers inflammatory cascades that exacerbate β cell demise. The current study focuses on UCP2, a mitochondrial inner membrane protein that has been implicated in regulating mitochondrial membrane potential and reactive oxygen species (ROS) production, ultimately affecting insulin secretion and cell viability.
The researchers employed a meticulously engineered nanomedicine platform capable of sequentially targeting β cell mitochondria within pancreatic islets. This strategic design ensures that the therapeutic agents are delivered precisely where they are needed, minimizing off-target effects and maximizing efficacy. By inhibiting UCP2 activity, the treatment disrupts the vicious cycle of mitochondrial dysfunction and autoinflammation, restoring cellular homeostasis. The study’s multidisciplinary approach, combining nanotechnology, molecular biology, and pharmacology, exemplifies the frontier of precision medicine in metabolic diseases.
.adsslot_ky25OSWp8t{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_ky25OSWp8t{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_ky25OSWp8t{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Delving deeper into the mechanistic insights provided by this research, the study reveals that UCP2 inhibition significantly reduces mitochondrial ROS generation, a key driver of the inflammatory response. Excess ROS not only damages mitochondrial DNA and proteins but also activates numerous pro-inflammatory signaling pathways within β cells. The novel nanomedicine demonstrates a remarkable ability to mitigate these effects, effectively curbing the autoinflammatory phenotype that leads to β cell apoptosis and dysfunction. This insight addresses a longstanding challenge in diabetes therapy — the direct protection and functional restoration of pancreatic β cells.
Innovation in targeted drug delivery underscored the success of this study. The nanomedicines are engineered to navigate the complex islet microenvironment delicately, utilizing surface modifications that recognize β cell-specific markers and mitochondrial membranes. This dual-targeting strategy ensures that therapeutic molecules penetrate deep into the mitochondria, the site of UCP2 action. Such specificity not only enhances therapeutic potential but also minimizes systemic toxicity, a critical consideration in treating chronic diseases such as T2DM where long-term safety is paramount.
The implications of this study extend beyond the immediate therapeutic effects. By eliminating autoinflammation in β cells, the intervention may halt or significantly slow the progression of T2DM, which often accelerates due to chronic low-grade inflammation. Autoinflammatory pathways are increasingly recognized as critical modulators of metabolic diseases, and the approach demonstrated here could serve as a blueprint for addressing similar mechanisms in other conditions. The concept of sequential nanomedicine targeting represents a paradigm shift, emphasizing temporal and spatial precision in drug delivery that matches the dynamic pathology of disease.
Critically, the research team provided compelling preclinical evidence showing that administration of the UCP2-targeted nanomedicine improves glucose homeostasis and insulin secretion in diabetic animal models. This functional restoration parallels observed reductions in inflammatory markers and mitochondrial distress within pancreatic islets, validating the therapeutic strategy’s multifaceted benefits. By preserving both β cell mass and function, this approach contrasts with current therapies focusing mainly on systemic glycemic control without directly addressing β cell health.
The study also explores the broader metabolic consequences of UCP2 inhibition, noting enhanced mitochondrial efficiency and improved cellular bioenergetics in treated β cells. These effects contribute to the normalization of insulin secretion dynamics, essential for maintaining glucose equilibrium. The findings position mitochondrial modulation not just as a secondary effect but as a primary therapeutic target in diabetes, challenging existing paradigms that have traditionally viewed β cell dysfunction as irreversible once established.
Furthermore, by integrating advanced nanotechnology with molecular targeting, this research exemplifies the potential of next-generation therapeutics to overcome the biological barriers that have hindered effective diabetes treatment. The biocompatible and biodegradable nature of the nanomedicines supports their clinical translation, addressing one of the key hurdles in nanomedicine development. The sophisticated yet scalable design promises adaptability to various mitochondrial targets and disease contexts, highlighting the versatility of this platform.
Importantly, this study also underscores the significance of dissecting β cell autoinflammation in the pathogenesis of T2DM. While systemic inflammation has been broadly acknowledged in diabetes, localized autoinflammatory processes within the islets have remained elusive targets. The successful targeting of mitochondrial dysfunction-induced autoinflammation offers a new lens through which to understand disease progression and design therapies that intervene earlier and more effectively.
Looking ahead, the researchers propose further exploration of combination therapies that may synergize with UCP2 inhibition, including antioxidants and anti-inflammatory agents tailored to the islet niche. Such combinatorial approaches could amplify therapeutic effects, fostering β cell regeneration and preserving endocrine function. Additionally, investigating the long-term outcomes and potential immunomodulatory effects of this intervention will be critical for clinical application.
The findings presented also invite a reevaluation of mitochondrial proteins and pathways as viable targets in metabolic diseases. UCP2’s dual role in regulating energy dissipation and ROS generation positions it uniquely at the intersection of metabolism and inflammation, making its precise modulation a promising strategy. The study’s demonstration of effective mitochondrial targeting highlights technological strides that can be leveraged to interrogate and manipulate other mitochondrial dysfunctions implicated in a spectrum of diseases.
This research heralds an exciting era of targeted nanomedicine in diabetes, where the convergence of molecular insight and engineering innovation unlocks new treatment horizons. By effectively ‘switching off’ detrimental mitochondrial signals driving autoinflammation, this approach reframes T2DM management from symptom control to root cause intervention. The potential to preserve β cell function and prevent disease progression carries profound implications for reducing the global diabetes burden.
As the global prevalence of T2DM continues to rise, the urgency for therapies that do more than manage symptoms has never been greater. This study’s nanomedicine-based strategy signals a crucial leap toward such transformative treatments. By addressing the cellular and subcellular derangements driving β cell failure, therapies emanating from this research could significantly enhance patient outcomes and quality of life.
In summary, the presented research elegantly combines molecular medicine and nanotechnology to target pancreatic β cell autoinflammation through UCP2 inhibition. The development of islet-mitochondrial sequential targeting nanomedicines not only elucidates a critical pathogenic mechanism but also offers a robust therapeutic avenue. This work promises to redefine diabetes treatment paradigms, emphasizing precision, safety, and the restoration of endogenous cellular function at the heart of metabolic disease.
Subject of Research:
Pancreatic β cell autoinflammation and mitochondrial dysfunction in type 2 diabetes mellitus with a focus on UCP2 inhibition using nanomedicine-based targeted therapy.
Article Title:
UCP2 inhibition eliminates pancreatic β cell autoinflammation in T2DM with islet-mitochondrial sequential targeting nanomedicines.
Article References:
Liu, Z., Chen, W., Zhang, J. et al. UCP2 inhibition eliminates pancreatic β cell autoinflammation in T2DM with islet-mitochondrial sequential targeting nanomedicines. Nat Commun 16, 6840 (2025). https://doi.org/10.1038/s41467-025-61883-y
Image Credits:
AI Generated
Tags: autoinflammation in pancreatic β cellsBlocking UCP2 in type 2 diabeteschronic insulin resistance in diabetesislet-mitochondrial targeting nanomedicinesmitochondrial health and β cell functionmitochondrial intervention in T2DMnovel approaches to diabetes treatmentprecision medicine in diabetes therapyreactive oxygen species and cell viabilityrole of UCP2 in insulin secretiontherapeutic strategies for T2DMβ cell inflammation and mitochondrial dysfunction