In a groundbreaking study published in Nature Communications, researchers have unveiled a novel therapeutic strategy targeting formyl peptide receptor-1 (FPR1) to combat lethal cutaneous drug reactions (LCDRs). These life-threatening skin conditions, often triggered by adverse drug reactions, have presented significant clinical challenges due to their rapid progression and limited treatment options. The innovative approach of inhibiting FPR1-mediated cell death offers newfound hope for patients suffering from these severe dermatological emergencies.
LCDRs encompass a spectrum of severe drug-induced skin disorders, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), characterized by widespread epidermal cell death and high mortality rates. Despite advancements in understanding their pathogenesis, therapeutic interventions remain largely supportive rather than curative. This research breakthrough stems from detailed mechanistic insights into the cellular signaling pathways underpinning these fatal reactions.
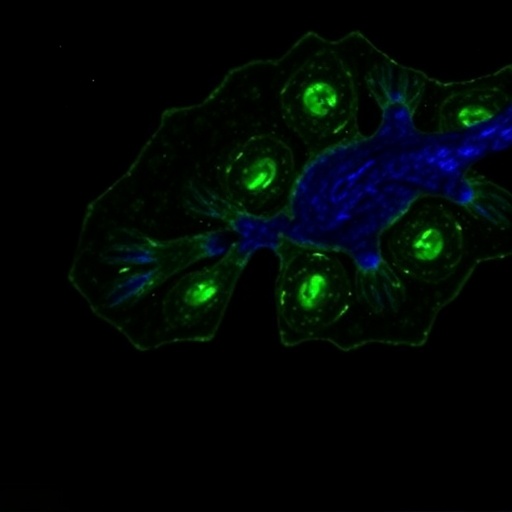
At the core of this study is the pivotal role of formyl peptide receptor-1, a G-protein coupled receptor extensively expressed on immune and epithelial cells. FPR1 functions as a sensor of mitochondrial damage-associated molecular patterns (DAMPs), particularly formylated peptides released by distressed cells. Upon activation, FPR1 triggers a cascade of intracellular events culminating in programmed necrosis or pyroptosis, amplifying tissue damage in affected skin.
Authors Kimura, H., Hasegawa, A., Nishiguchi, T., and colleagues performed comprehensive preclinical experiments elucidating how blockade of FPR1 could mitigate this necrotic cell death and thereby curb the progression of fatal skin lesions. Using in vitro models of keratinocyte injury and in vivo murine models mimicking human LCDRs, they demonstrated that pharmacological inhibition or genetic knockdown of FPR1 significantly reduced epidermal cell loss and improved survival outcomes.
The mechanistic investigations revealed that FPR1 activation instigates downstream signaling via the MAPK and NF-kB pathways, provoking pro-inflammatory gene expression and caspase-independent cell death modalities. By intercepting this receptor’s activity, the researchers effectively halted the deleterious feedback loop of inflammation and necrosis that characterizes SJS/TEN pathology. This finding represents a transformative shift from mere symptomatic care to targeted molecular intervention.
What distinguishes this study is the targeted nature of the therapeutic inhibition. The team utilized small-molecule antagonists specifically designed to bind FPR1 with high affinity, reducing off-target effects commonly associated with broader immunosuppressants. These antagonists not only attenuated receptor activation but also preserved normal immune vigilance, a crucial balance to avoid increased susceptibility to infections.
Further, by employing advanced imaging and biomarker analyses, the study delineated the spatial and temporal patterns of FPR1 expression and engagement within lesions. This precise mapping underscored the dynamic interplay between damaged keratinocytes and infiltrating immune cells, revealing a localized microenvironment conducive to sustained FPR1-mediated cytotoxicity. Interrupting this interaction thus emerged as a key therapeutic axis.
A notable aspect of this research involved the translational validation of findings. Patient-derived skin samples from individuals with acute LCDRs exhibited heightened FPR1 expression correlating with lesion severity, affirming the clinical relevance of targeting this receptor. This alignment between experimental and human data strengthens the case for advancing FPR1 inhibitors into early-phase clinical trials.
Moreover, the study explores the safety profile of FPR1 antagonism. Preclinical toxicology assessments indicated minimal adverse effects on systemic immune functions and the absence of off-target cytotoxicity, addressing critical hurdles in drug development. Longitudinal observation in animal models corroborated sustained therapeutic benefits without compromising host defense mechanisms.
This pioneering work not only directs attention to an underappreciated receptor in dermatopathology but also opens avenues for personalized medicine approaches in managing drug hypersensitivity reactions. Stratifying patients by FPR1 expression or genetic polymorphisms may optimize treatment responsiveness, tailoring interventions to individual risk profiles.
The potential clinical impact extends beyond lethal cutaneous drug reactions. Given FPR1’s involvement in various inflammatory and immune-mediated conditions, the therapeutic paradigm proposed here could inform broader applications in autoimmune diseases, chronic wound healing, and even cancer biology where similar necrotic pathways contribute to pathology.
The interdisciplinary collaboration between immunologists, dermatologists, pharmacologists, and molecular biologists underpins the robust nature of this discovery. By integrating cutting-edge cell biology, receptor pharmacology, and translational medicine, the research exemplifies the modern scientific approach required to tackle complex clinical challenges.
As the global medical community continues to grapple with the burden of drug-induced skin toxicity, innovations like FPR1 inhibition offer a beacon of hope. The promise of turning deadly dermal reactions into manageable conditions reflects a leap forward in patient care and exemplifies the transformative power of targeted molecular therapies.
Future directions will likely focus on optimizing drug candidates for human use, elucidating detailed receptor-ligand interactions, and expanding the scope of preclinical models. Close clinical monitoring and biomarker development will be critical to monitor therapeutic efficacy and personalize dosing regimens, ensuring maximal benefit with minimal risk.
The study’s insights into receptor-mediated necrosis challenge conventional dogma and highlight the intricate molecular dialogues dictating cell fate in inflammatory milieu. Such groundbreaking revelations underscore the necessity of continuous innovation in understanding receptor biology as a gateway to novel therapeutic landscapes.
In conclusion, the inhibition of FPR1 represents an exciting frontier in the treatment of lethal cutaneous drug reactions, combining precision medicine with a deep mechanistic understanding of cell death pathways. This advancement not only offers tangible clinical benefits but also sets a precedent for future research endeavors aiming to mitigate drug-induced toxicities worldwide.
Subject of Research: Investigation of the role and therapeutic targeting of formyl peptide receptor-1 (FPR1) in lethal cutaneous drug reactions.
Article Title: Inhibition of formyl peptide receptor-1-mediated cell death as a therapy for lethal cutaneous drug reactions in preclinical models.
Article References: Kimura, H., Hasegawa, A., Nishiguchi, T. et al. Inhibition of formyl peptide receptor-1-mediated cell death as a therapy for lethal cutaneous drug reactions in preclinical models. Nat Commun 16, 8708 (2025). https://doi.org/10.1038/s41467-025-63744-0
Image Credits: AI Generated
Tags: cell death in dermatological emergenciesFPR1 inhibition for drug-induced skin reactionsG-protein coupled receptor signalinginnovative therapies for severe skin conditionslethal cutaneous drug reactions treatmentmechanisms of drug-induced skin damagemitochondrial damage and skin healthNature Communications study on skin reactionsprogrammed necrosis and pyroptosisStevens-Johnson syndrome researchtherapeutic strategies for skin disorderstoxic epidermal necrolysis prevention