A team led by engineers at the University of California San Diego has developed a biodegradable polymer system to treat rheumatoid arthritis, an autoimmune and inflammatory disease, by working in concert with the power of the human immune system.
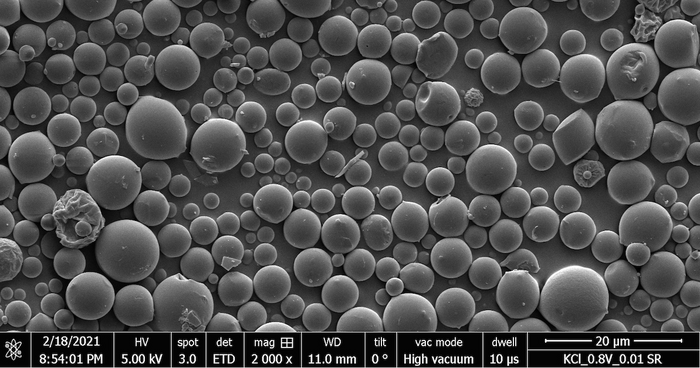
Credit: David McBride, UC San Diego
A team led by engineers at the University of California San Diego has developed a biodegradable polymer system to treat rheumatoid arthritis, an autoimmune and inflammatory disease, by working in concert with the power of the human immune system.
The research builds on increasing clinical interest in modulating the immune system to treat cancers and autoimmune disease, as well as previous work with all-trans retinoic acid (ATRA) which is produced naturally in the body and helps cells grow and develop. By approaching these challenges from the perspective of a biomaterials engineering lab, the team adds two key innovations to previous methods: local release and harnessing the joint microenvironment for sustained effectiveness.
With this method, encapsulated ATRA is injected directly into a joint affected by rheumatoid arthritis, where it remains in effect for at least several weeks. During that time, ATRA transforms disease-causing cells into disease-stopping cells, known as regulatory T cells, which can treat or prevent the disease elsewhere in the body.
“Essentially, our system turns the disease site into a factory that produces regulatory T cells,” said David A. McBride, a chemical engineering graduate student at UC San Diego supervised by nanoengineering professor Nisarg Shah. “It uses a biodegradable biomaterial to facilitate the timed release of ATRA, which reprograms T cells so they can treat disease.”
The research was published in the March 8, 2023 issue of Advanced Science. McBride is a coauthor on the paper.
“This is a very promising line of research utilizing the latest and greatest technology in immunoengineering to combat arthritis,” said Iannis Adamopoulous, an associate professor of medicine at Harvard’s Beth Israel Deaconess Medical Center, Department of Medicine, Division of Rheumatology.
What is ATRA?
ATRA is a small molecule currently FDA approved to treat acute promyelocytic leukemia (APML). Research over the last two decades has suggested that it also has promise in treating autoimmune arthritis and relieving inflammation. However, that method relies on ATRA traveling freely throughout the body, which can cause immunosuppression and potentially significant off-target toxicity, along with other unwanted side effects.
“Previous work established that ATRA has potential in treating autoimmune arthritis, but the route of administration precluded the work from being relevant to clinical translation,” said McBride.
When ATRA is encapsulated using biodegradable materials, it can be injected directly into joints at therapeutic concentrations but as it diffuses out of the joint, it enters circulation at much lower concentrations, minimizing or preventing unwanted effects. Without the controlled release afforded by the biomaterial encapsulation, patients would require multiple injections per day to achieve the same effects, which would be impractical in most cases.
How it works
When the human immune system functions properly, helper T cells patrol the body in search of disease-causing pathogens. When a pathogen is detected, a helper T cell can recruit additional cells to help fight it. “It’s kind of similar to how you might have police cars roaming the city, and when one sees a crime occurring, they call for backup to get the situation under control,” said McBride.
Many autoimmune diseases result from cases of “mistaken identity,” in which these cells attack a perceived danger target that is in fact a part of normally functioning cells in the body. The subsequent proliferation of such pathogenic T cells, which McBride calls “bad apples,” can result from a combination of genetic and environmental factors and wreak havoc on the body when they summon large teams of immune cells for unnecessary standoffs.
For example, “in type 1 diabetes, you have bad apples that call in reinforcements against your pancreas,” said McBride. ”In multiple sclerosis, it is against your neurons. In rheumatoid arthritis, it is against your joints. So, your immune system recognizes this as something to be attacked, and it goes and recruits a bunch of additional immune cells to these places and fights a war until all the pathogens are gone. Except that, in this case, it’s not attacking pathogens, but healthy parts of the body.”
Many current approaches block the chemical signals that immune cells use to communicate, effectively preventing the pathogenic T cells from calling in reinforcements without eliminating the “bad apples.” Time-released ATRA reprograms them to act as regulatory T cells, or “good apples.” These cells still have the ability to recognize and activate in the joints, but rather than calling in additional immune cells, they help to resolve the inflammation. In areas such as joints, which aren’t recommended for repeated injections, the sustained-release formulation allows sufficient therapeutic exposure to flip the balance.
ATRA makes lasting modifications to the ability of cellular machinery to read cell DNA, improving the function of the anti-inflammatory regulatory T cells. This treats T cells at the site of disease and generates regulatory T cells specific to that diseased tissue. Then, when these cells move to other disease locations, they can help resolve inflammation and promote healing. Because the cells are specific to the disease, they don’t interfere with normal immune function, allowing them to supplement existing therapies or provide alternatives for patients who need them.
“The coolest part about this is that the treated site of disease, where the bad apples were previously proliferating, now becomes a place that can generate regulators that can now go patrol the body and actually prevent disease,” said McBride.
The limitations of existing approaches
Patients with rheumatoid arthritis are frequently treated with disease-modifying anti-rheumatic drugs (DMARDs) and in many patients this approach works well. However, about a third of patients don’t adequately respond to front-line DMARDs, and they come with some significant disadvantages.
First, while using DMARDs, some patients become more susceptible to infectious disease and exhibit weaker responses to vaccines. In this regard, “the COVID-19 pandemic has brought a lot more understanding on the risks of immunosuppression into public awareness,” said McBride.
Additionally, because most immunosuppressives currently used to treat rheumatoid arthritis stay in the system for up to two weeks, there is no option to discontinue treatment if a dangerous infection occurs. This is compounded when patients use two or more treatments simultaneously, which is not uncommon due to the complexity of the disease. Using multiple powerful immunosuppressants can exacerbate the risks of infections or cancer.
“If you can instead have a treatment option that doesn’t have an immunosuppressive effect, you can really reduce the risk for patients that need multiple treatment modalities to keep their autoimmune disease in check,” McBride said.
Finally, for some patients, immunosuppressives work well for a time and then lose their effectiveness. This can happen when their bodies develop antibodies that neutralize the medications or new disease pathways emerge. New treatments like this one could potentially supplement DMARDs, compensating for waning effectiveness or requiring lower doses to start with.
“In well controlled patients, reducing or eliminating the need for immunosuppressive drugs is desirable,” said Shah. “However, when it is attempted, studies have shown that the disease can flare up again. So having a non-immunosuppressive option could go a long way.”
Research methods, challenges and next steps
The team tested its biomaterial-encapsulation method using a combination of mouse and human cells. After this achieved positive results, they transitioned to mouse models of autoimmune arthritis, coming closer to simulating the remarkable complexity of a real-life case of autoimmune disease in a human subject.
The work required multiple models of disease, each designed to demonstrate a specific aspect of the team’s hypothesis, as well as rigorously tracking the cells from their origin points at injection to the other locations where they recirculated and proved effective in fighting disease.
Currently, the researchers are actively working toward commercialization. “As this is my first experience with something like this, it is difficult for me to estimate, but we are currently targeting approval to start clinical trials within five years,” said McBride. To evaluate possible commercialization routes, McBride has participated in the UC San Diego Institute for the Global Entrepreneur (IGE) NSF I-Corps and MedTech Accelerator programs.
The power of a multidisciplinary approach
When he entered graduate school at UC San Diego, McBride was focused on modeling complex signaling patterns in biological systems, for which rheumatoid arthritis provided many intriguing examples. He became more engaged as he gained awareness of the human side of the disease.
“I’m always surprised at how many people know someone fighting an autoimmune disease or are struggling with one themselves,” he said. “These experiences have really moved it from an interesting problem on paper that I’m trying to solve to a real, difficult problem in the lives of friends and family,”
This research required a highly interdisciplinary approach, relying on input from experts in biomaterials design, immunology, clinical rheumatology and beyond. McBride credits the highly collaborative environment on the UC San Diego campus as a crucial factor in its success.
“UC San Diego doesn’t only promote academic collaboration, but also provides several resources for translating our discoveries beyond the lab and into the clinic,” he said. “Most recently, we are excited to have been awarded a UC San Diego internal grant under the Accelerating Innovations to Market program.”
Shah, McBride and paper co-senior author Nunzio Bottini, MD, PhD, a former Professor of Medicine at UC San Diego, now with Cedars-Sinai Medical Center, received the Accelerating Innovation to Market (AIM) award for 2023. “By including high-caliber industry and investment experts in the selection process, it provides precious validation of the commercial potential of our idea,” Bottini said. “Plus, it supports the laboratory in completing proof of concept validation work needed to accelerate translation.”
Paper: Immunomodulatory microparticles epigenetically modulate T cells and systemically ameliorate autoimmune arthritis
Coauthors: David A. McBride and Matthew D. Kerr, Department of Nanoengineering and Chemical Engineering Program, UC San Diego; Wade T. Johnson, Department of nanoengineering, UC San Diego; Anders Nguyen, Department of Rheumatology and Inflammation Research, Sahlgrenska Academy, Institute of Medicine, University of Gothenburg, Sweden; Martina Zoccheddu, Department of Medicine, Division of Rheumatology, Allergy and Immunology, UC San Diego; Mina Yao and Edward B. Prideaux, Department of Chemistry and Biochemistry, UC San Diego; Nicholas C. Dorn, Department of Nanoengineering and Chemical Engineering Program, UC San Diego; Wei Wang, Department of Chemistry and Biochemistry and Department of Cellular and Molecular Medicine, UC San Diego; Mattias N.D. Svensson, Department of Rheumatology and Inflammation Research, Sahlgrenska Academy, Institute of
Medicine, University of Gothenburg, Sweden; Nunzio Bottini*, Department of Medicine, Division of Rheumatology, Allergy and Immunology, UC San Diego; and Nisarg J. Shah*, Department of Nanoengineering and Chemical Engineering Program, UC San Diego.
*These are corresponding authors.
Sources of funding for the research include:
- National Institutes of Health grant F31AR079921 (DAM)
- National Institutes of Health grant F31HL164055 (MDK)
- National Institutes of Health grant T32AR064194
- National Institutes of Health grant T32CA153915
- National Institutes of Health grant P30AR073761 (NB)
- National Institutes of Health grant R03DE031009 (NJS)
- National Institutes of Health grant S10OD025052
- National Institutes of Health grant P30CA23100
- National Institutes of Health grant UL1TR001442
- National Science Foundation grant ECCS-2025752
- National Psoriasis Foundation (NJS)
- Arthritis National Research Foundation (NJS)
- Hellman Fellowship (NJS)
- Swedish Society for Medical Research (SSMF) grant S19-0062 (MNDS)
- Foundation for Research in Rheumatology (MNDS)
- IngaBritt och Arne Lundbergs Forskningsstiftelse (MNDS)
Journal
Advanced Science
Article Title
Immunomodulatory microparticles epigenetically modulate T cells and systemically ameliorate autoimmune arthritis
Article Publication Date
8-Mar-2023



