Credit: James McNew/Rice University
HOUSTON — (June 28, 2018) — James McNew's and Michael Stern's biochemical hunt for the root cause of a rare, paralyzing genetic disorder is a 10-year quest that's taken an unexpected turn toward everyday killers such as Alzheimer's disease, cancer and aging.
The National Institutes of Health has awarded the Rice University scientists a five-year R01 grant to investigate a biochemical domino effect that begins with a critical regulatory protein called TOR and ends with cells dying of oxidative stress. TOR regulates cell growth and survival and only recently became a focus for Stern and McNew, professors of biochemistry and cell biology in Rice's Department of BioSciences and co-investigators on the $1.9 million grant from the NIH's National Institute of Neurological Disorders and Stroke.
"It's known that TOR controls starvation in virtually every animal, including humans," McNew said. "Decreased TOR activity has even been found to increase the life span of yeast, worms and fruit flies, and some studies have found that TOR-inhibiting drugs increase the life span of mice. Increased TOR activity is also involved in cancer and has been implicated in Alzheimer's, Parkinson's and other neurodegenerative diseases, including one called hereditary spastic paraplegia (HSP) that we have studied for many years."
HSP, a rare disorder that affects about 20,000 people in the U.S., is marked by numbness and weakness in the legs and feet due to progressive deterioration of the longest cells in the body — the neurons that connect the spine to the lower legs.
In 2016 Stern, McNew and colleagues used hundreds of experiments on dozens of mutant strains of fruit flies to show how an HSP gene produced defective synapses at the junctions between nerve and muscle cells. In follow-up work last year, McNew, Stern and postdoctoral researcher Shiyu Xu conducted more experiments to see exactly how these synapse defects caused neurons to malfunction and die.
"Shiyu wasn't able to find any evidence of neurodegeneration, but he did find evidence of muscle degeneration," Stern said. "That was a surprise, and we didn't know what to make of it at first. Even though nerve damage is a known cause of muscle atrophy, conventional wisdom is that the nerve cells die first."
Intrigued, the group conducted experiments to see what was happening at the molecular level. Tests suggested elevated TOR activity in the degenerating muscle cells. TOR is short for "target of rapamycin"; when TOR was discovered in the early 1990s, researchers only knew it was the target of a natural compound called rapamycin, an immunosuppressant that had been widely prescribed for decades to transplant recipients.
"We were convinced it was TOR after Shiyu showed he could slow down the muscle degeneration by giving the flies rapamycin," Stern said.
TOR is an important master regulator of growth and nutrient-sensing. When fully activated, TOR promotes growth so aggressively that cells forgo daily chores such as repairing structural damage and recycling partially functional organelles. In times of extreme stress or starvation, TOR is fully deactivated so the cell can enter a survival mode and conserve scarce resources.
"TOR isn't an on-off switch as much as a knob for dialing growth up or down," McNew said. "It's not that high TOR is bad and low TOR is good. Each is needed under certain conditions, and TOR's function — which is essential in all higher-order life, from yeast to humans — is to modulate growth to match the conditions it's detecting."
Stern said, "What appears to be happening in the muscle cells that aren't receiving neuronal signals is that the knob gets switched onto high and stays there. TOR locks the cells into this aggressive, pro-growth mode and they stop cleaning up all of the reactive oxygen species, or free radicals, which gradually build up and cause such high levels of stress that the cell dies."
Stern said this hypothesis jibes with observations from numerous other studies that have found high TOR levels and high levels of oxidative stress in the brain cells of patients with Alzheimer's as well as the atrophied muscles of patients who are paralyzed or bedridden.
"In muscle atrophy studies in mice, where the motor neuron is cut, they've found that TOR is activated," he said. "This might be mechanistically similar to our case or to what's been seen in Alzheimer's because people have also found activation of the stress pathway that's induced by reactive oxygen species."
Stern said previous studies also have identified some of the molecular players involved in the degeneration domino effect — including two proteins known as the JNK kinase and the FOXO transcription factor — but he and McNew are the first to connect the dots between TOR and the stress-pathway proteins.
"We also see FOXO activation in our degeneration model, but we know — or at least we think we know — what is activating FOXO," Stern said. "We hypothesize that TOR causes a buildup of reactive oxygen species that in turn activates a molecule called JNK, which activates FOXO."
McNew said focusing on the damage from overactive TOR means that any clues he and Stern find could potentially apply to any disease or condition in which TOR activation is implicated.
"The things that cause TOR to get turned on in a neuron are probably very different than those that turn it on in a liver cell or a white blood cell," he said. "We're focused on the downstream part because once you get TOR turned on, we think it does a handful of things we understand and can directly test. And those are likely to be uniform across different cell types and different conditions. That means anything we find could inform not only HSP pathology but also cancer and neurodegenerative diseases like Alzheimer's and Parkinson's."
###
High-resolution IMAGES are available for download at:
http://news.rice.edu/files/2018/06/0625_TOR-toon-lg-1mc68er.jpg
CAPTION: At a healthy synapse (top), neuron-muscle communication (thick green arrow) prevents TOR activation in muscle, permitting repair of cellular structures and muscle survival. Synapse defects (bottom) from HSP mutations and other neuronal disorders disrupt this communication (thin green arrow), which activates TOR protein in the muscle, allowing junk proteins to build up and cause muscle degeneration and ultimately death. (Image courtesy of James McNew/Rice University)
http://news.rice.edu/files/2018/06/0625_TOR-jmms7-lg-13612k5.jpg
CAPTION: Rice University biochemists Michael Stern (left) and James McNew are co-investigators on a new five-year grant from the National Institute of Neurological Disorders and Stroke to study how an overactive regulatory protein called TOR can lead to cell death from oxidative stress. (Photo by Jeff Fitlow/Rice University)
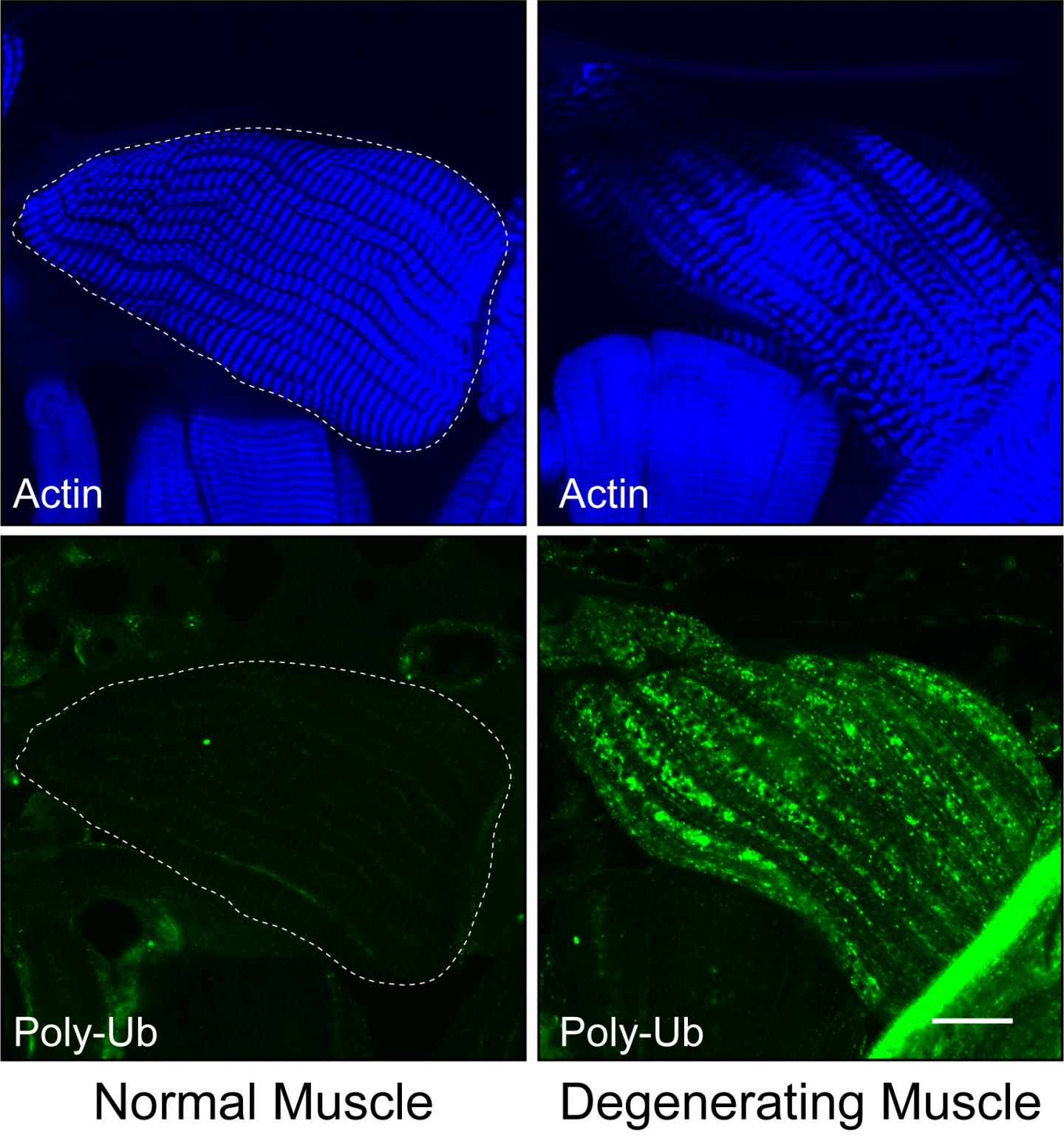
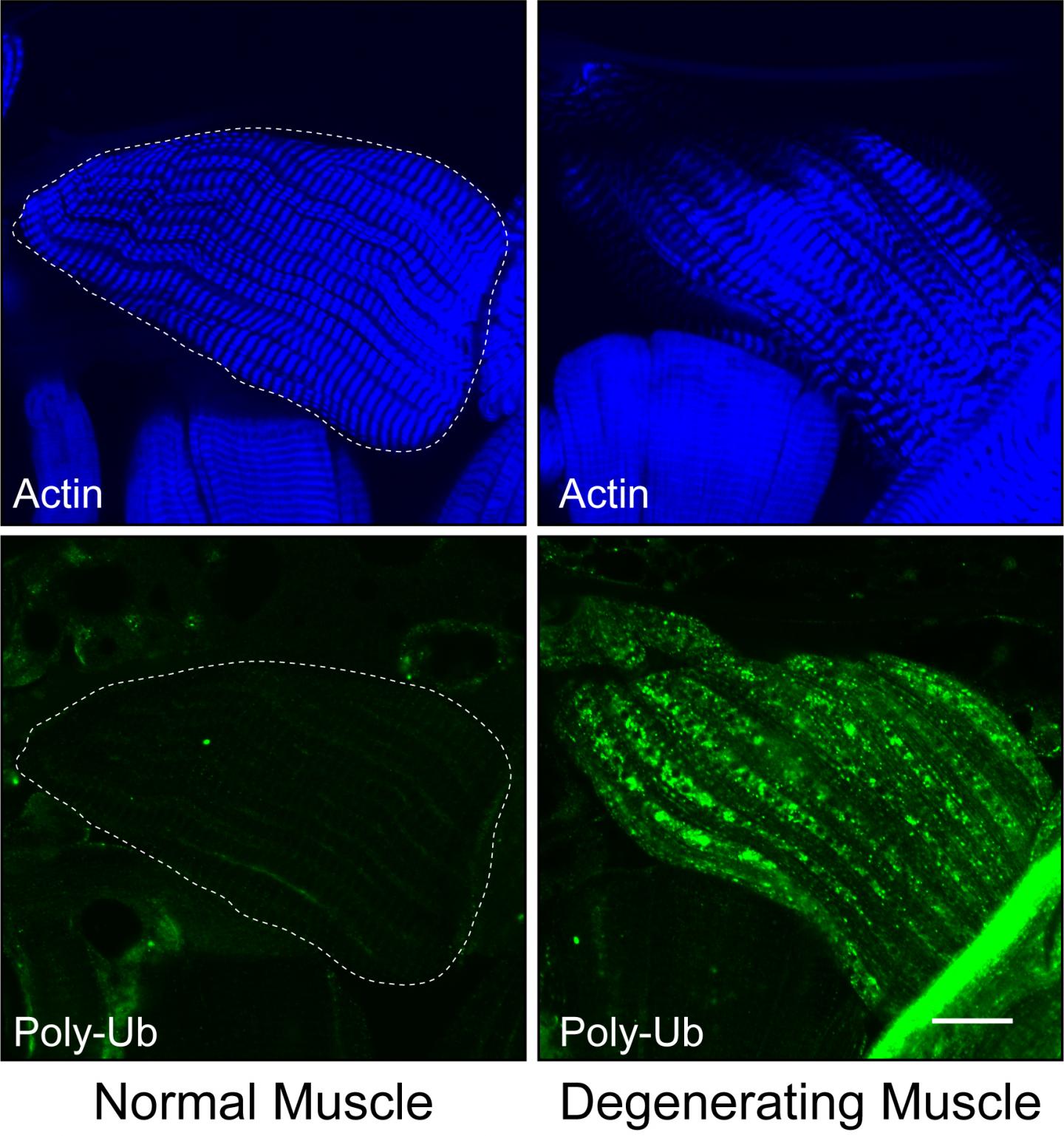
http://news.rice.edu/files/2018/06/0625_TOR-fig-lg-2g86rhc.jpg
CAPTION: In microscopic images of muscle tissue from normal fruit flies (left), fluorescent tags reveal uniform levels of the structural protein actin (blue) and almost no poly-UB, a protein aggregate that is broken apart and recycled by healthy cells. In muscle tissue from flies lacking HSP gene activity (right), actin levels are reduced and cells contain a toxic buildup of poly-UB. (Image courtesy of James McNew/Rice University)
http://news.rice.edu/files/2018/06/0625_TOR-stern18-lg-22e452j.jpg
CAPTION: Michael Stern is a professor of biochemistry and cell biology in Rice University's Department of BioSciences. (Photo by Jeff Fitlow/Rice University)
http://news.rice.edu/files/2018/06/0625_TOR-McNew9-lg-zeiths.jpg
CAPTION: James McNew is a professor of biochemistry and cell biology in Rice University's Department of BioSciences. (Photo by Jeff Fitlow/Rice University)
A copy of the NIH grant abstract is available at: http://bit.ly/2yQQLx1
Related research stories from Rice:
Rice bioscientists show how HSP genes affect neurotransmission — April 4, 2016 http://news.rice.edu/2016/04/04/rice-bioscientists-show-how-hsp-genes-affect-neurotransmission/
Researchers probe protein linked to hereditary spastic paraplegia — Oct. 8, 2012 http://news.rice.edu/2012/10/08/researchers-probe-protein-linked-to-hereditary-spastic-paraplegia/
Research proposes common link between autism, diabetes — Oct. 20, 2011 http://news.rice.edu/2011/10/20/research-proposes-common-link-between-autism-diabetes-2/
Study offers new clues about hereditary spastic paraplegia — July 8, 2011 http://news.rice.edu/2011/07/08/study-offers-new-clues-about-hereditary-spastic-paraplegia/
Little-known protein found to be key player — July 29, 2009 http://news.rice.edu/2009/07/29/little-known-protein-found-to-be-key-player/
Researcher tracks path of genetic disease — Feb. 1, 2007 http://news.rice.edu/2007/02/01/researcher-tracks-paths-of-genetic-disease/
This release can be found online at news.rice.edu.
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation's top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 3,970 undergraduates and 2,934 graduate students, Rice's undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for quality of life and for lots of race/class interaction and No. 2 for happiest students by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger's Personal Finance. To read "What they're saying about Rice," go to http://tinyurl.com/RiceUniversityoverview.
Media Contact
Jade Boyd
[email protected]
713-348-6778
@RiceUNews
http://news.rice.edu