In recent scientific developments, a groundbreaking study has unveiled new insights into the therapeutic potential of basic fibroblast growth factor (BFGF) in the context of ovarian cytotoxicity induced by chemotherapeutic agents. The research, prominently conducted by a team including Li, Zhang, and Lv, investigates the molecular mechanisms behind how BFGF interacts with critical signaling pathways to protect ovarian cells from damage caused by chemotherapy. This significant endeavor opens new avenues for safeguarding reproductive health in patients undergoing cancer treatment.
The study primarily focuses on the detrimental effects of chemotherapeutic agents, specifically cyclophosphamide (CTX), which has long been known to pose risks to ovarian health. CTX is a cornerstone in cancer treatment but comes with a considerable downside, often leading to ovarian failure or infertility. As the battle against cancer intensifies, preserving the reproductive capabilities of patients remains a pivotal concern, especially among younger women diagnosed with the disease. The research highlights how BFGF can serve as a protective agent against such adverse effects, shedding light on its potential roles in fertility preservation.
One of the striking revelations of the research is the involvement of the SERPINE1/HIF-1 and Nrf-2/HO-1 signaling pathways in mediating the effects of BFGF. The intricate interplay of these pathways had remained relatively unexplored in the context of ovarian toxicity. SERPINE1, a serine protease inhibitor, has been recognized for its role in cellular processes such as proliferation, migration, and apoptosis, particularly in cancer biology. The research illuminates how BFGF elevates SERPINE1 levels, thereby triggering protective mechanisms to counteract the cytotoxic effects sustained from CTX administration.
Another facet of this study emphasizes the significance of hypoxia-inducible factor 1 (HIF-1). This master regulator of cellular responses to low oxygen levels plays a crucial role in tumor biology and has protective effects on various tissues. By modulating the expression of HIF-1 through BFGF, it is suggested that ovarian cells can enhance their resilience against chemotherapy-induced damage, paving the way for targeted therapeutic interventions that prioritize patient safety and quality of life during treatment.
The Nrf-2/HO-1 signaling pathway also garners considerable attention in this research, recognized for its critical role in cellular defense mechanisms against oxidative stress. Chemotherapeutic agents often induce oxidative stress, a contributing factor to cellular damage and apoptosis. The confirmation that BFGF can activate Nrf-2 and subsequently increase HO-1 expression provides compelling evidence for its potential use in clinical settings to ameliorate the adverse effects of CTX.
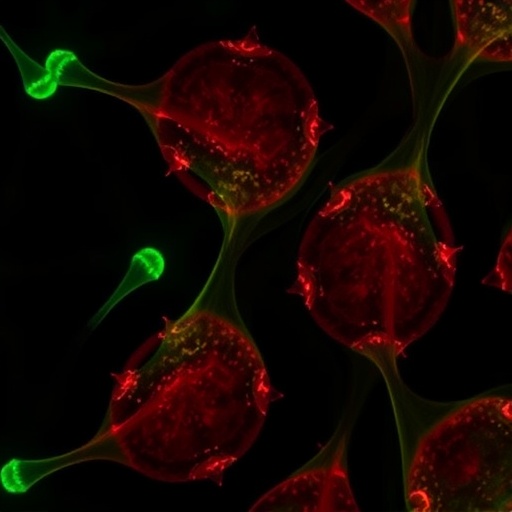
What sets this study apart is not just the identification of these signaling pathways but also the meticulous approach taken to validate the findings. The researchers employed a variety of experimental designs, including in vitro assays using ovarian cell lines and in vivo studies utilizing animal models. This multifaceted methodology strengthens the evidence supporting BFGF’s protective effects and provides a robust foundation for future clinical applications.
The broader implications of this research extend beyond oncology; they touch upon reproductive health, fertility preservation, and personalized medicine. As cancer treatments continue to evolve, integrating a fertility-preserving strategy alongside traditional chemotherapy regimens could dramatically change the landscape for many patients. The findings from Li, Zhang, and Lv could inspire innovative treatment paradigms that not only aim for complete cancer remission but also prioritize preserving a woman’s ability to conceive post-treatment.
Furthermore, the study prompts a critical discussion on the future of integrating growth factors like BFGF in therapeutic protocols. As the medical field steers towards more tailored approaches to cancer treatment, understanding the biological mechanisms at play becomes imperative. This research not only elucidates the protective role of BFGF but also sets the stage for further investigations into similar agents that can mitigate the side effects of life-saving therapies.
With BFGF now highlighted as a potential ally in the fight against chemotherapy-induced ovarian toxicity, the research beckons for follow-up studies. It raises pertinent questions about dosage, long-term effects, and how BFGF can be safely incorporated into clinical practices. Such inquiries will be essential for translating laboratory results into real-world solutions that can be widely implemented in oncology.
Moreover, the research ignites hope for patients and advocates for continued support of studies aimed at women’s health. As pressure mounts on healthcare systems to provide comprehensive cancer care that respects patients’ lives beyond mere survival, the findings underscore the need for a holistic approach to treatment. Achieving a balance between effective cancer management and maintaining reproductive health could redefine care protocols and ultimately transform survivor experiences.
As we venture into this promising landscape of fertility preservation amidst oncology, the study serves as a benchmark for future research endeavors. With ongoing investigations into the signaling pathways implicated in ovarian protection and the potential for novel therapies, the field remains poised to push the boundaries of what is possible.
In conclusion, the pioneering work by Li and colleagues not only champions the cause of protecting ovarian health during chemotherapy but also sparks a wider discourse on personalized medicine. The imminent need for synergistic approaches that harmonize cancer treatment and reproductive health is more critical now than ever. This intersection of research and compassion may deliver a paradigm shift in the way oncologists consider treatment plans, ultimately leading to better health outcomes and quality of life for patients.
The study of BFGF’s involvement in mitigating CTX-induced ovarian cytotoxicity is a clarion call to the scientific community. As we stand at the forefront of innovation in cancer therapies, let this research inspire a brighter outlook for future generations confronting cancer, with the promise of life and health unlimited by the shadow of treatment adversities.
Subject of Research: The protective role of basic fibroblast growth factor (BFGF) in ovarian cytotoxicity induced by chemotherapy.
Article Title: BFGF mitigates CTX-induced ovarian cytotoxicity via SERPINE1/HIF-1 and Nrf-2/HO-1 signaling pathways.
Article References: Li, Y., Zhang, L., Lv, H. et al. BFGF mitigates CTX-induced ovarian cytotoxicity via SERPINE1/HIF-1 and Nrf-2/HO-1 signaling pathways. J Ovarian Res 18:151 (2025). https://doi.org/10.1186/s13048-025-01736-w
Image Credits: AI Generated
DOI:
Keywords: BFGF, ovarian cytotoxicity, chemotherapy, SERPINE1, HIF-1, Nrf-2, HO-1, reproductive health, cancer treatment, fertility preservation.
Tags: basic fibroblast growth factor researchBFGF ovarian protectioncancer treatment and fertilitychemotherapy toxicity on ovariescyclophosphamide side effectsfertility preservation in cancer patientsNrf-2 HO-1 signaling mechanismsovarian cytotoxicity preventionreproductive health during chemotherapySERPINE1 HIF-1 interactionsignaling pathways in ovarian healththerapeutic potential of BFGF