In the relentless pursuit to understand and exploit the vulnerabilities of cancer cells, researchers have uncovered an intricate interplay between the immune signaling pathways and genetic defects that could redefine therapeutic strategies against notoriously difficult-to-treat cancers. A groundbreaking study recently published in Nature Communications shines light on an unexpected mechanism by which cancers harboring mutations in the BRCA1 or BRCA2 genes become exquisitely sensitive to disruptions in a key RNA-editing enzyme, ADAR1. This discovery not only deepens our understanding of cancer biology but also highlights a promising synthetic lethal approach with potentially far-reaching implications for targeted cancer therapies.
BRCA1 and BRCA2 mutations have long been established as pivotal players in hereditary breast and ovarian cancers, impairing the cells’ ability to repair DNA double-strand breaks through homologous recombination. This deficiency predisposes cells to genomic instability and tumorigenesis yet simultaneously generates peculiar susceptibilities that can be therapeutically exploited. Traditionally, inhibitors of PARP enzymes have leveraged such vulnerabilities by further crippling DNA repair. However, resistance to PARP inhibitors often emerges, underscoring the dire need for alternative avenues to selectively eradicate BRCA-deficient tumors.
The research team, led by Chabanon and colleagues, has identified a surprising source of synthetic lethality tied to ADAR1—a crucial RNA-editing enzyme responsible for converting adenosine residues to inosine on double-stranded RNA (dsRNA). ADAR1’s activity is essential in attenuating innate immune responses by modulating the recognition of endogenous dsRNA species, preventing inappropriate activation of antiviral pathways. The study elucidates how the absence or inhibition of ADAR1 in BRCA1/2-mutant cancers triggers an autocrine interferon response so severe that it effectively poisons the cancer cells from within, leading to their demise.
.adsslot_AmHCeZwkTl{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_AmHCeZwkTl{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_AmHCeZwkTl{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Through comprehensive molecular and cellular analyses, the investigators demonstrated that impairing ADAR1 in BRCA1/2-deficient models resulted in the accumulation of unedited dsRNA, thereby activating the cytosolic RNA sensors MDA5 and PKR. The ensuing signaling cascade culminated in a robust autocrine production of type I interferons, which not only amplified the immune-stimulatory environment but also induced a toxic feedback loop detrimental to the cancer cells themselves. This interferon poisoning acts as a lethal blow, overwhelming the defective BRCA-mutant cells, a phenomenon absent or significantly attenuated in BRCA-proficient contexts.
Crucially, this work delineates the molecular framework underlying this synthetic lethal interaction. The researchers employed gene-editing tools to inactivate ADAR1 selectively, observing that the resultant cellular stress and interferon induction only manifested lethality in cells lacking functional BRCA1 or BRCA2. This specificity underscores a compelling therapeutic window, as normal cells or tumors without these mutations retain sufficient buffering capacity against the interferon toxicity elicited by ADAR1 suppression.
Moreover, the dual role of interferon signaling here is both fascinating and intricate. While interferons are classically viewed as key mediators of antiviral defense and immune activation, their excessive autocrine production can paradoxically become cytotoxic. The study posits that in BRCA-mutant cancer cells, the baseline genomic instability and compromised DNA repair machinery exacerbate susceptibility to the pro-apoptotic and stress-inducing effects of heightened interferon signaling, effectively turning the cell’s own immune sensome against itself.
This research also broadens our understanding of how cancer cells evade innate immunity and the potential Achilles’ heels therein. The ADAR1 enzyme functions as a critical modulator to prevent aberrant immune activation—a safeguard that BRCA-mutant cancers exploit for survival. By undermining this protective shield through ADAR1 inhibition, the study reveals a novel angle to provoke lethal autoimmunity within malignant cells, bypassing traditional immune checkpoint mechanisms and potentially overcoming resistance to immunotherapy.
From a therapeutic perspective, the implications are profound. Targeting ADAR1 pharmacologically could represent a next-generation strategy to selectively poison BRCA1/2-mutant tumors, especially those refractory to existing treatments. The synthetic lethal paradigm carved out by these findings offers promise for precision medicine, where exploiting the unique vulnerabilities of cancer cells minimizes collateral damage to normal tissues and mitigates adverse effects.
Future translational efforts will undoubtedly focus on developing potent and selective ADAR1 inhibitors, optimizing delivery methods to tumor sites, and integrating this approach with existing modalities such as PARP inhibitors and immune checkpoint blockers. The documented interferon-mediated autocrine toxicity could also serve as a biomarker to gauge therapeutic response and tailor treatment regimens dynamically.
The study’s rigorous integration of biochemical assays, RNA sequencing, and functional genomics advances a nuanced model illustrating how defects in DNA repair converge with dysregulated RNA editing and innate immune sensing. It also raises captivating questions about the broader roles of ADAR1 and interferon signaling in cancer and immune homeostasis, setting the stage for a new chapter in tumor immunology.
One cannot overlook the potential that such discoveries hold in expanding the arsenal against cancers that have historically evaded curative interventions. The dual vulnerability exploited here—combining inherent DNA repair deficiencies with the intrinsic immune regulatory circuitry—may open avenues to not only overcome drug resistance but also minimize the window for cancer escape mechanisms.
Beyond therapeutic innovation, this work underscores the intricate balance cells maintain between sustaining genomic integrity and modulating immune responses. It reveals how the perilous interplay of RNA editing and antiviral defense mechanisms can be harnessed against malignant cells, reflecting the elegant complexity of cellular systems where each molecular cog interlocks with another, shaping fate and function.
In essence, Chabanon and colleagues’ research vividly illustrates the power of synthetic lethality to transform cancer biology understanding and treatment. By revealing how autocrine interferon poisoning mediated by ADAR1 loss unleashes a lethal vulnerability in BRCA1/2-mutant cancers, it paves the way for novel therapeutic strategies that could translate into improved survival and quality of life for patients burdened by these aggressive malignancies.
As the scientific community digests these findings, the challenge and excitement lie in bridging the gap from bench to bedside. Clinical trials evaluating ADAR1 inhibition in BRCA-mutant cancers will be eagerly anticipated, with hopes that this mechanistic insight will soon catalyze tangible benefits in oncology practice.
In the grand scheme, the interplay between RNA editing, immune activation, and DNA repair as revealed here underscores a paradigm shift, prompting researchers and clinicians alike to consider cancer vulnerabilities beyond static genetic lesions, embracing dynamic cellular processes as therapeutic targets.
This breakthrough underscores once again how the converging paths of molecular biology, immunology, and genomics continue to dismantle cancer’s defenses, bringing us closer to therapies tailored with surgical precision and mechanistic sophistication.
Subject of Research: Synthetic lethality in BRCA1/2-mutant cancers via ADAR1-dependent autocrine interferon signaling
Article Title: Autocrine interferon poisoning mediates ADAR1-dependent synthetic lethality in BRCA1/2-mutant cancers
Article References:
Chabanon, R.M., Shcherbakova, L., Lacroix-Triki, M. et al. Autocrine interferon poisoning mediates ADAR1-dependent synthetic lethality in BRCA1/2-mutant cancers. Nat Commun 16, 6972 (2025). https://doi.org/10.1038/s41467-025-62309-5
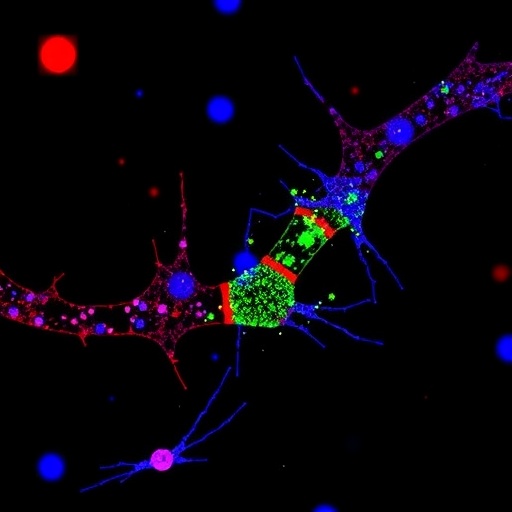
Image Credits: AI Generated
Tags: ADAR1 synthetic lethalityAutocrine interferon signalingBRCA1 and BRCA2 mutationscancer biology advancementsgenomic instability in cancerhereditary breast and ovarian cancersimmune signaling pathways in cancernovel cancer treatment strategiesPARP inhibitor resistanceRNA-editing enzyme vulnerabilitiestargeted cancer therapiestherapeutic exploitation of cancer weaknesses