Credit: Dr. Giuseppe Madonia, Dr. Ursula Madonia and Bentham Science Publishers
The privilege to operate in a specialist asthma clinic allows for a light to be shed on the persistence of the many pitfalls in the management of this condition, which continue despite the recommendations of the numerous authoritative guidelines produced and spread in the last decades. Asthma heterogeneity and variability make it extremely difficult to be optimally managed, also in a specialist environment.
Many factors contribute to overcomplicate things: correct diagnosis and, if necessary, a differential one (e.g. COPD, vocal cord disfunction, congestive heart failure, emotional dyspnea, for example); characterization and education of the so-called poor perceiver; creation of a partnership with the patient; etc…
In other words, it is necessary to spend time on every single patient and his/her particular form of asthma and to formulate a more or less stringent plan of follow-up. That being said, it appears clear how the role of physicians is particularly challenging in managing comfortably this complexity and the burden produced by it. Overcoming these obstacles will be the result of knowledge, dedication, constancy and acquired experience. A recent National Institute for Health and Care Excellence (NICE) guideline suggests the best practice in asthma management directly to general practitioners assuming however that "putting recommendations into practice can take time".(1)
Almost all patients with a suspect of asthma will have their first evaluation in a primary care setting (2). But a single general practitioner physician will not regularly observe, in his daily practice, such a patient. Concurrently, it is unclear how many spirometry tests he will do in a month: possibly not enough to guarantee an acceptable level of expertise in such a key role test (3,4). It will likely be very difficult to acquire the optimal background level appropriate to smoothly manage asthma condition – especially in such a busy, diverse and eclectic environment (5).
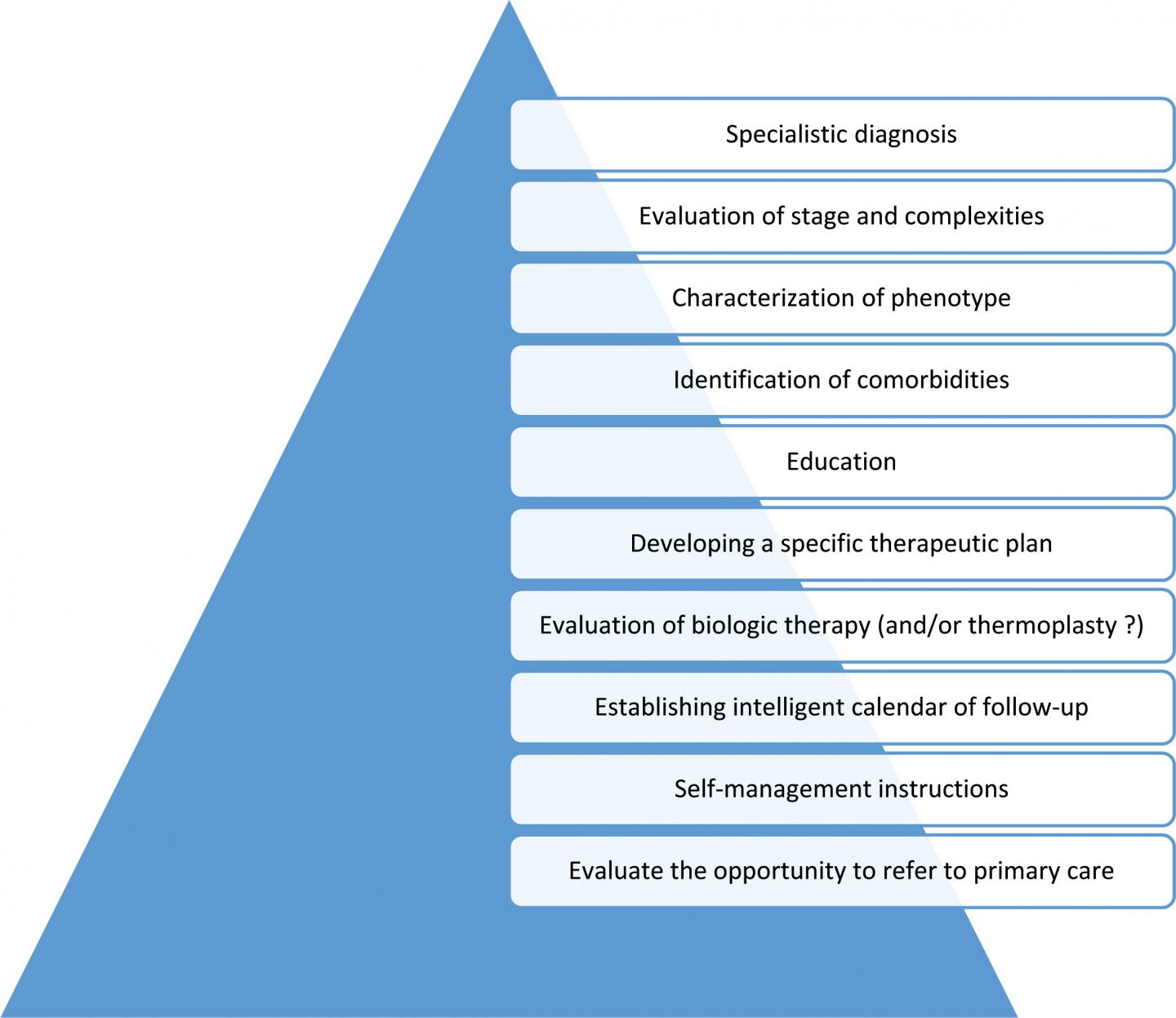
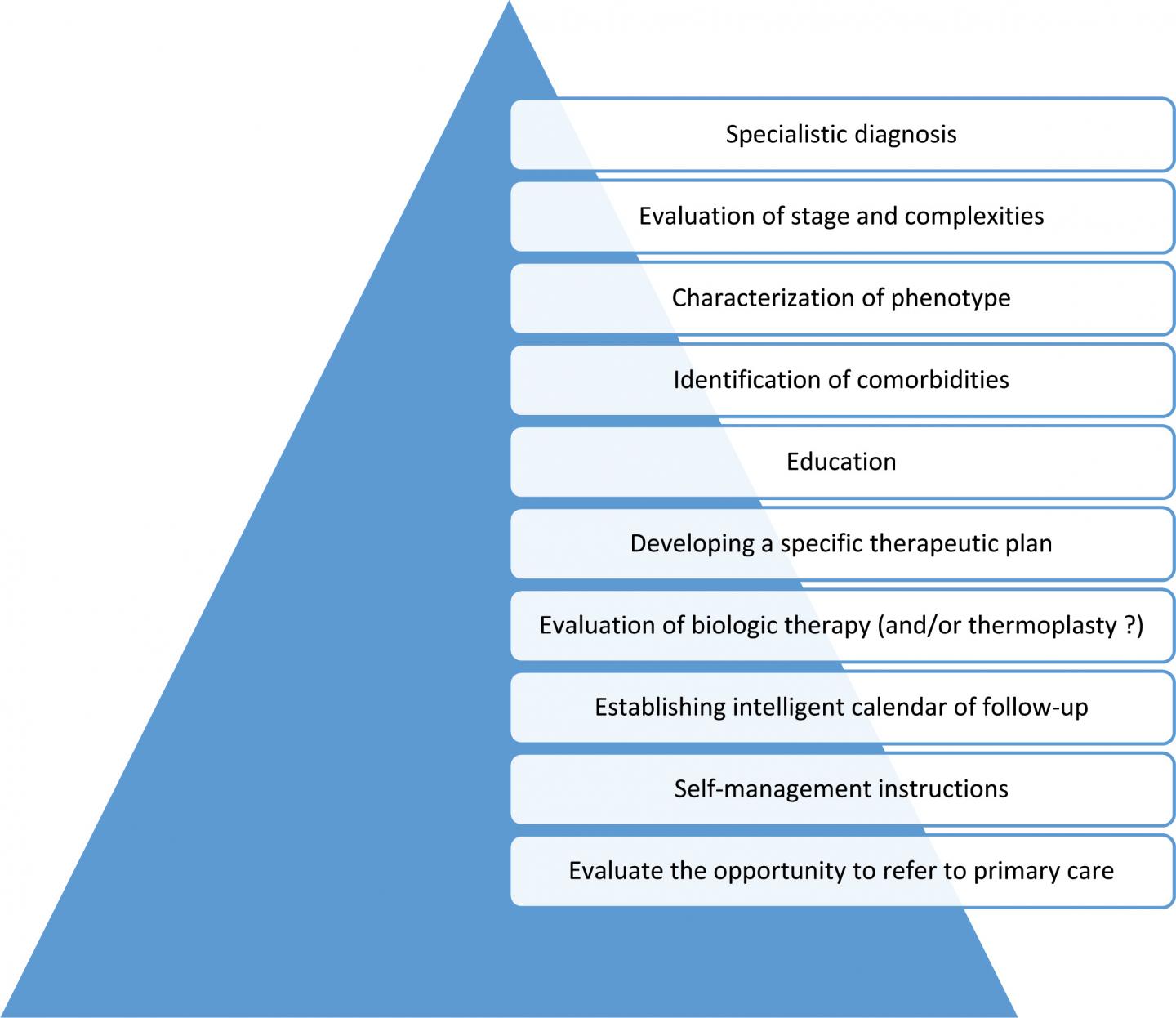
The few considerations just briefly exposed make it reasonable to assume that, paradoxically, it could be better, in future guidelines on the topic, to typify when a respiratory physician – taking into account the local health system – can refer an asthmatic patient to the primary care colleague (and not vice versa) (6).
###
For further information on the research study, please visit: http://www.eurekaselect.com/160581
References:
1) Asthma: diagnosis, monitoring and chronic asthma management. Nice guideline. 29 November 2017.
2) Wechsler ME , "Managing Asthma in Primary Care:Putting New Guideline Recommendations Into Context" Mayo Clin Proc. 2009;84(8):707-717
3) E. Derom, C. van Weel, G. Liistro, et al. "Primary care spirometry " Eur Respir J 2008; 31: 197-203
4) Hegewald MJ, Gallo HM, and Wilson EL "Accuracy and Quality of Spirometry in Primary Care Offices" Ann Am Thorac Soc Vol 13 2016, No 12, 2119-2124,
5) Bosnic-Anticevich SZ "Asthma management in primary care: caring, sharing and working together" Eur Respir J 2016; 47: 1043-1046
6) Price D,Bjermer L, Bergin DA, Martinez R " Asthma referrals: a key component of asthma management that needs to be addressed" Journal of Asthma and Allergy 2017:10 209-223
Media Contact
Faizan ul Haq
[email protected]
@BenthamScienceP
http://benthamscience.com/
Related Journal Article
http://dx.doi.org/10.2174/1573398X14666180320124324