In the evolving field of cardiovascular medicine, the integration of mechanical circulatory support devices (MCSDs) has become paramount for patients suffering from severe heart conditions. Despite their lifesaving potential, these devices present unique challenges, particularly in the realm of platelet dysfunction. Awareness of this dysfunction and its monitoring is crucial, as it plays a pivotal role in patient outcomes. Recent research has shed light on the key markers and detection methods used to evaluate platelet dysfunction specifically in patients with MCSDs. This opens a new horizon in understanding how to manage and mitigate the risks associated with such technologies.
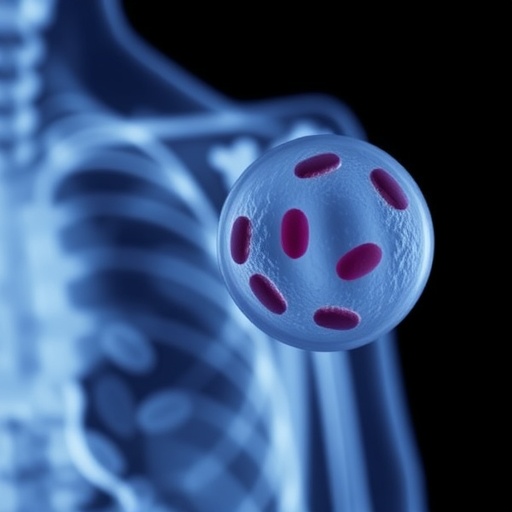
Platelet dysfunction in patients using mechanical circulatory support devices is characterized by a decreased ability of platelets to aggregate and form proper clots, which is vital for normal hemostasis. This dysfunction can lead to serious complications, such as bleeding or thromboembolism, which can offset the benefits of the mechanical devices designed to support cardiac function. Researchers like Wei, Li, and Su are leading efforts to identify specific biomarkers that indicate platelet dysfunction, providing a foundation for better monitoring and intervention strategies.
As these devices circulate blood mechanically, they can induce shear stress and other conditions that adversely affect platelet function. The mechanical process often causes structural changes in platelets, leading to altered reactivity. As clinicians and researchers delve deeper into the biochemical pathways affected by these devices, a clearer picture of the underlying causes of platelet dysfunction is emerging, which can inform future treatment strategies.
To date, several key markers have been identified that can reliably indicate the presence of platelet dysfunction in patients utilizing MCSDs. These markers can vary based on the type of device, patient demographics, and clinical context, underscoring the complexity of diagnosing dysfunction. Research indicates that biomarkers such as soluble P-selectin, platelet-derived microvesicles, and various other cytokines can serve as reliable indicators of platelet activity and dysfunction in these patients.
Detection methods for monitoring these biomarkers continuously evolve, with advancements in technology facilitating more nuanced assessments. Techniques like flow cytometry, which analyzes the physical and chemical characteristics of cells or particles, have become integral in evaluating platelet function. Additionally, biomarkers can be quantified using enzyme-linked immunosorbent assays (ELISAs) and other biochemical assays. These methods allow for high-throughput analysis, making it easier for clinicians to keep pace with the monitoring demands of patients on MCSDs.
Importantly, the timing of assessments plays a critical role in accurately gauging platelet function. Research has revealed that platelet dysfunction may fluctuate over time, influenced by factors such as device usage duration and patient health status. Thus, establishing optimal monitoring intervals is vital for patient safety and efficacy. Continuous monitoring systems are being explored to allow real-time evaluation, significantly enhancing patient care and allowing for timely therapeutic interventions.
In addition to identifying markers and developing detection methods, research has emphasized the relationship between device materials and platelet activation. Certain materials used in MCSDs may have inherent properties that trigger platelet activation and dysfunction, complicating the therapeutic landscape. Investigating biocompatibility and surface modifications of these devices could lead to advancements that minimize platelet activation, thereby improving patient outcomes.
The insights gained from ongoing research are not merely academic; they hold profound implications for clinical practice. By integrating these findings into routine assessments, healthcare providers can develop more personalized treatment plans. This enhanced capability allows for tailored management strategies that consider the unique challenges presented by mechanical circulatory support devices, significantly optimizing patient care.
Moreover, understanding the mechanisms of platelet dysfunction could pave the way for innovative therapeutic approaches, including pharmacologic interventions that target specific pathways or utilize agents that enhance platelet function. The potential to develop personalized medicine strategies based on an individual’s unique profile of platelet activity is particularly exciting, ushering in an era of more effective management of patients reliant on mechanical circulatory support.
As more research continues to elucidate the relationship between platelet dysfunction and mechanical circulatory support, the academic and clinical communities are urged to collaborate in harmonizing findings within the broader cardiovascular healthcare framework. Cross-disciplinary partnerships could accelerate the translation of laboratory findings into clinical applications, benefitting patient outcomes and shaping the future of cardiac care.
In conclusion, the work of Wei, Li, and Su highlights essential aspects of platelet dysfunction in the context of mechanical circulatory devices. Their identification of pertinent biomarkers and detection methodologies represents a significant advancement in the quest to improve patient management strategies. As these insights continue to inform clinical practices, the goal remains to enhance the quality of life for patients relying on such vital interventions, ultimately bridging the gap between technology and compassionate patient care.
While platelet dysfunction represents a formidable challenge in the use of mechanical circulatory support devices, the growing body of research on effective monitoring and management strategies gives hope. As these strategies evolve and improve, it is crucial that the medical community remains vigilant, using evidence-based approaches to enhance patient safety and outcomes.
This ongoing dialogue in the realms of research and clinical application will be vital for future advancements, ensuring that the use of mechanical circulatory support devices aligns with the highest standards of patient care and safety. Ultimately, the health of patients with severe cardiac conditions may depend on our ability to accurately identify and manage platelet dysfunction arising from their mechanical support systems.
Subject of Research: Platelet Dysfunction in Mechanical Circulatory Support Devices
Article Title: Key markers and detection methods for evaluating platelet dysfunction in mechanical circulatory support devices.
Article References:
Wei, Z., Li, Z., Su, W. et al. Key markers and detection methods for evaluating platelet dysfunction in mechanical circulatory support devices.J Artif Organs (2025). https://doi.org/10.1007/s10047-025-01520-z
Image Credits: AI Generated
DOI: 10.1007/s10047-025-01520-z
Keywords: Platelet dysfunction, mechanical circulatory support devices, biomarkers, detection methods, cardiovascular medicine.
Tags: biomarkers for platelet dysfunctioncardiovascular medicine advancementscomplications of mechanical circulatory supportevaluating platelet function in heart failure patientshemostasis challenges in circulatory supportintervention strategies for platelet dysfunctionmonitoring platelet function in cardiac patientspatient outcomes with MCSDsplatelet dysfunction in mechanical circulatory support devicesresearch on platelet aggregationshear stress impact on plateletsthromboembolism risks in heart device patients