A groundbreaking systematic review and meta-analysis has unveiled critical insights into the complex and life-threatening phenomenon of apnoea in preterm neonates. Presented by Chen, Zandvoort, Baxter, and colleagues in the prestigious journal Pediatric Research, this comprehensive study meticulously quantifies the relationships between apnoea duration and the ensuing cardiorespiratory and cerebrovascular responses in this vulnerable population. The research shines a spotlight on the physiological perturbations that occur as apnoea episodes lengthen, providing vital information that could revolutionize clinical approaches to neonatal care.
Apnoea of prematurity, characterized by the cessation of breathing for extended periods, represents a significant and pervasive challenge faced by neonatologists worldwide. Premature infants, whose respiratory control systems are inherently immature, frequently experience these apneic events, which can culminate in life-threatening hypoxia and bradycardia. Despite decades of clinical observation, the nuanced interplay between the duration of apnoea and the body’s compensatory mechanisms remains inadequately characterized—until now.
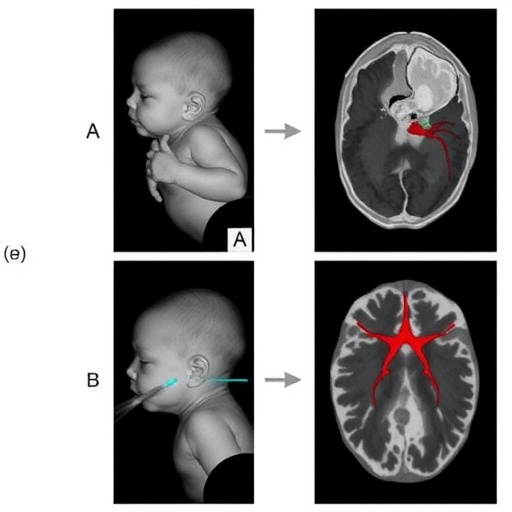
Through exhaustive data synthesis gathered from numerous observational studies and clinical trials, this investigation offers an unprecedented meta-analytical perspective on how varying lengths of apnoeic episodes modulate cardiorespiratory and cerebrovascular dynamics. Notably, as apnoea duration escalates, the research identifies significant decrements in oxygen saturation and heart rate, coupled with alterations in cerebral blood flow, which collectively threaten neonatal homeostasis. These insights highlight crucial windows during which interventions may be most efficacious.
One of the pivotal observations from the meta-analysis is the nonlinear behavior of cardiorespiratory responses relative to apnoea length. Initial short apnoeic episodes trigger adaptive reflexes aimed at preserving oxygen delivery and maintaining cerebral perfusion. However, as the duration extends beyond critical thresholds, the compensatory mechanisms become overwhelmed, leading to precipitous declines in systemic and cerebral oxygenation. This biphasic response underscores the urgency for timely clinical detection and intervention.
The cerebrovascular consequences of prolonged apnoea, as detailed in the study, elucidate a potential mechanistic pathway contributing to the neurological vulnerabilities frequently observed in preterm infants. Fluctuations in cerebral blood flow during apnoea may precipitate ischemic injury or exacerbate the risk of intraventricular hemorrhage, conditions with long-term developmental implications. Understanding these pathophysiological shifts is imperative for developing targeted therapies that minimize neurodevelopmental morbidity.
Importantly, the authors articulate the heterogeneity inherent in the analyzed studies, drawing attention to variations in study design, patient demographics, and measurement methodologies. Despite these variabilities, the meta-analysis robustly delineates trends that remain consistent across diverse clinical environments, reinforcing the validity of its conclusions. This rigorous methodological approach enhances confidence in translating findings into practice.
The study also explores how external factors such as gestational age, the presence of comorbidities, and therapeutic interventions modulate the relationship between apnoea and cardiorespiratory outcomes. Such stratified analyses offer nuanced understanding that could inform personalized medicine strategies, optimizing monitoring and treatment protocols tailored to individual risk profiles.
Clinically, the implications of this meta-analysis are profound. By establishing quantitative thresholds where apnoea-induced physiological disruptions become critical, healthcare providers can refine criteria for respiratory support initiation, such as continuous positive airway pressure or pharmacological stimulation. Early detection through advanced monitoring technologies, coupled with evidence-based intervention timing, promises to improve survival and neurological outcomes significantly.
Furthermore, the research invites a reevaluation of current monitoring paradigms, emphasizing the integration of multimodal approaches tracking both cardiac and cerebral parameters concurrently. The dynamic cerebrovascular changes highlighted stress the necessity for technologies capable of continuous cerebral oxygenation and perfusion monitoring alongside traditional cardiorespiratory indicators.
On a broader scope, this work propels forward the scientific understanding of neonatal respiratory control mechanisms. By mapping the trajectory of physiological responses during apnoea, it opens avenues for innovative research into the neurochemical and autonomic pathways governing respiratory drive and vascular regulation in preterm infants.
Moreover, the meta-analysis strengthens the imperative for interdisciplinary collaboration among neonatologists, neurologists, and biomedical engineers. The complex pathophysiology unraveled necessitates integrative strategies combining clinical insight, technological advancements, and neurodevelopmental expertise to mitigate the devastating consequences of apnoea in this delicate patient group.
Ultimately, the findings serve as a clarion call for enhanced vigilance and tailored clinical protocols to address apnoea’s multifaceted impacts. The systematic accumulation and synthesis of evidence presented by Chen et al. establish a new benchmark in neonatal care research, charting a course toward improved outcomes through informed, precise, and timely intervention.
As healthcare systems grapple with the burden of prematurity-related complications worldwide, this study’s insights arrive as an invaluable resource guiding policy and practice reforms. It underscores the critical need for investment in neonatal monitoring infrastructure, staff training, and research to translate these scientific revelations into tangible health benefits.
In conclusion, the meticulous work of Chen and colleagues illuminates the intricate physiological landscape of apnoea duration and its cardiocerebral ramifications in preterm neonates. This landmark meta-analysis moves the field closer to unraveling the complexities of neonatal respiratory pathophysiology and offers a robust evidence base to underpin next-generation clinical strategies. The implications for reducing morbidity and mortality in this fragile population are both profound and promising, heralding a future where science and technology intricately safeguard the earliest stages of human life.
Subject of Research: Apnoea duration and its impact on cardiorespiratory and cerebrovascular responses in preterm neonates.
Article Title: Apnoea duration and changes in cardiorespiratory and cerebrovascular responses in preterm neonates: a systematic review and meta-analysis.
Article References:
Chen, Y., Zandvoort, C.S., Baxter, L. et al. Apnoea duration and changes in cardiorespiratory and cerebrovascular responses in preterm neonates: a systematic review and meta-analysis. Pediatric Research (2025). https://doi.org/10.1038/s41390-025-04496-x
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04496-x
Tags: apnoea in preterm neonatescardiorespiratory changes in neonatescerebrovascular responses in infantsclinical approaches to apnoea of prematurityhypoxia and bradycardia in preterm infantsmeta-analysis of neonatal apnoeaneonatal care advancementsneonatal respiratory control systemsobservational studies on neonatal healthphysiological effects of apnoeasystematic review on apnoeaunderstanding apnoea duration effects