Severe acute pancreatitis (SAP) remains one of the most formidable challenges in clinical medicine, given its complex pathological cascade and the profound systemic complications that often accompany the condition. Characterized by an abrupt and intense inflammatory response, SAP not only devastates the pancreas itself but frequently precipitates multi-organ damage, including critical injury to the lungs, liver, and kidneys. Recent research out of Lin, S., Liang, F., Chen, C., and colleagues has shed illuminating new light on the molecular players that regulate inflammation in acute pancreatitis. At the center of this groundbreaking work lies Annexin A1 (Anxa1), a glucocorticoid-regulated protein long reputed for its potent anti-inflammatory effects in various contexts. This study offers a deep dive into the precise role that Anxa1 performs within the immune microenvironment of acute pancreatitis, opening exciting avenues for therapeutic innovation.
Acute pancreatitis unfolds as a paradox of immune hyperactivity and tissue destruction. The initial injury triggers an explosion of inflammatory signals, predominantly orchestrated by innate immune cells such as myeloid lineage populations, including macrophages and neutrophils. These cells infiltrate the pancreas and release cytokines, chemokines, and reactive oxygen species, which amplify local damage and can extend injury beyond the pancreas. Understanding how these immune responses are regulated—particularly how excessive inflammation is curtailed—has been an unmet need in pancreatitis research. The study by Lin et al. focuses on Anxa1, which functions as a critical physiological brake on inflammation, to unravel how this protein affects the trajectory of severe acute pancreatitis.
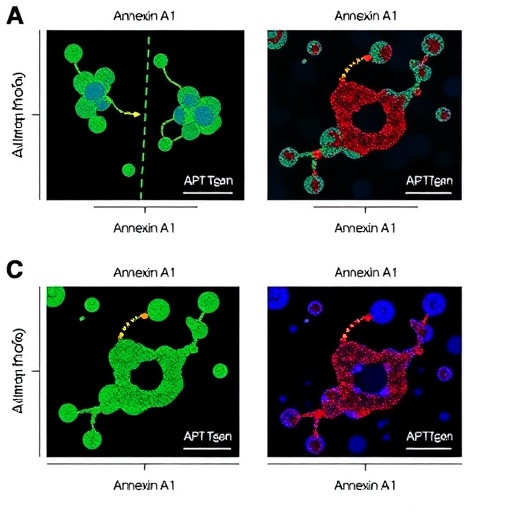
Using sophisticated, cutting-edge methodologies, the researchers employed flow cytometry to quantify cellular populations expressing Anxa1 throughout the course of pancreatitis. Complementing this, single-cell RNA sequencing provided a high-resolution view of gene expression programs activated within distinct myeloid cell subsets during disease progression. By integrating these technologies, they captured the dynamic regulation of Anxa1 in an unprecedented manner. Their data revealed a striking pattern: while Anxa1 expression is initially upregulated in early-phase myeloid cells in response to injury, a subsequent decline or deficiency in Anxa1 compromises the host’s ability to control rampant inflammation.
To probe causality, the investigators turned to animal models, including Anxa1 knockout mice, to dissect the consequences of Anxa1 loss during SAP. The absence of Anxa1 led to exacerbated pancreatic damage typified by increased necrosis, edema, and inflammatory cell infiltration. More alarmingly, these mice displayed amplified systemic inflammatory responses that culminated in severe injury to extra-pancreatic sites such as the lungs, liver, and kidneys. This finding highlights the integral role that Anxa1 plays not only locally within the pancreas but also in restraining widespread immune activation that underpins multi-organ dysfunction syndrome (MODS) in SAP.
In parallel, the study explored intervention strategies by administering Ac2-26, a synthetic peptide derived from the N-terminal domain of Anxa1 known to mimic its biological activity. Treatment with Ac2-26 markedly ameliorated the severity of pancreatic injury as well as systemic inflammation, demonstrating therapeutic promise. This peptide effectively dampened neutrophil infiltration and cytokine storms, fostering a resolution phase conducive to tissue repair. Such findings suggest that Anxa1-based therapies could be harnessed to modulate immune responses and improve clinical outcomes in SAP, a condition currently lacking targeted pharmacological treatments.
The implications of these observations ripple through the field of immunology and gastroenterology. Anxa1 emerges as a critical immunomodulatory checkpoint that calibrates the intensity of myeloid cell-mediated inflammation during pancreatic injury. By maintaining a delicate balance between necessary defense mechanisms and excessive immune-driven damage, Anxa1 prevents the vicious cycle of escalating inflammation that leads to systemic organ failure. This protein’s regulation appears to be tightly controlled, with glucocorticoids potentially orchestrating its expression—a link that opens possibilities for synergistic therapeutic strategies.
Notably, this work underscores the importance of the myeloid compartment as both an effector and regulator of inflammation in SAP. The single-cell transcriptomic analyses enabled identification of specific myeloid subpopulations that dynamically alter Anxa1 levels in response to tissue injury cues. These nuanced insights into immune cell heterogeneity and plasticity add a new layer of complexity to our understanding of pancreatitis pathogenesis and highlight specialized targets for intervention.
Furthermore, the study confronts the challenge of systemic inflammation as a chief contributor to SAP mortality. By demonstrating that loss of Anxa1 aggravates injury in vital organs beyond the pancreas, it emphasizes the interconnectedness of local pancreatic pathology and systemic immune dysregulation. Treatment paradigms that reinforce Anxa1 function could therefore not only protect the pancreas but also mitigate multi-organ complications that often dictate patient prognosis.
The methodological rigor employed—ranging from state-of-the-art flow cytometry to single-cell RNA profiling—strengthens the study’s conclusions and elevates its impact. This multi-angled approach enables a granular understanding of cellular dynamics within a complex inflammatory milieu. The translational relevance is especially exciting; synthetic peptides like Ac2-26 have tangible clinical appeal owing to their well-defined mechanisms and capacity for controlled delivery.
Another notable aspect is the study’s alignment with the growing appreciation of lipid-mediated resolution pathways in inflammation. Annexin A1 and its derivatives are part of a broader class of pro-resolving mediators that actively terminate inflammation and prompt tissue repair. Integrating such endogenous pathways into therapeutic design represents a paradigm shift that moves beyond immunosuppression toward restoration of immune homeostasis.
From a clinical perspective, the identification of Anxa1 as a therapeutic target heralds a potential leap forward in SAP management. Given the high morbidity and mortality rates associated with SAP, novel interventions that blunt excessive inflammation without compromising host defense are urgently needed. The translational pipeline from bench to bedside could be expedited by leveraging peptides like Ac2-26, which have established safety profiles in preclinical models.
In summary, Lin et al.’s landmark study intricately dissects the role of Annexin A1 in severe acute pancreatitis, establishing it as a key regulator that tempers inflammatory responses and shields both the pancreas and distal organs from injury. By unveiling the detrimental consequences of Anxa1 deficiency and the therapeutic efficacy of its mimetic peptide, the research charts a compelling course for the development of targeted anti-inflammatory strategies in SAP. This advancement promises not only to deepen our molecular understanding of pancreatitis but also to transition into impactful clinical therapies that improve patient outcomes.
As the medical community continues to grapple with the complexities of SAP, insights from this study highlight the necessity of balanced immune regulation and the power of harnessing endogenous anti-inflammatory mediators. Future research building on these findings may extend to human trials and exploration of Anxa1’s role in other inflammatory diseases, broadening its clinical relevance. Amidst evolving paradigms in immunomodulation, Annexin A1 stands out as a guardian protein that holds the key to unlocking new therapeutic possibilities.
This pioneering work underscores the intricate interplay between immune cells and resident tissue during acute pancreatitis and presents a natural shield system that can be therapeutically exploited. In doing so, it paves the way towards revolutionizing the treatment landscape of SAP, translating complex molecular insights into tangible patient benefits.
Subject of Research: Annexin A1’s role in regulating inflammatory-immune response and tissue injury in severe acute pancreatitis.
Article Title: Annexin A1 regulates inflammatory-immune response and reduces pancreatic and extra-pancreatic injury during severe acute pancreatitis.
Article References:
Lin, S., Liang, F., Chen, C. et al. Annexin A1 regulates inflammatory-immune response and reduces pancreatic and extra-pancreatic injury during severe acute pancreatitis. Genes Immun 26, 124–136 (2025). https://doi.org/10.1038/s41435-025-00321-x
Image Credits: AI Generated
DOI: April 2025
Tags: Annexin A1 role in inflammationanti-inflammatory effects of Annexin A1chemokines and immune signalingcytokines in acute pancreatitisglucocorticoid-regulated proteinsimmune response in pancreatitismacrophages in pancreatitismulti-organ damage in pancreatitisneutrophils and tissue damagepancreatic inflammation and injurysevere acute pancreatitis mechanismstherapeutic targets for pancreatitis