In the rapidly evolving field of cancer immunotherapy, a newly published study in Nature Communications from 2026 has shed groundbreaking light on how different types of radiopharmaceuticals distinctly influence immune responses when paired with immune checkpoint inhibitors. Authored by Kerr, Jin, Liu, and colleagues, this research dissects the nuanced immunological mechanisms triggered by alpha- and beta-particle emitting radiopharmaceuticals, providing critical insights that could revolutionize therapeutic strategies against resistant tumors.
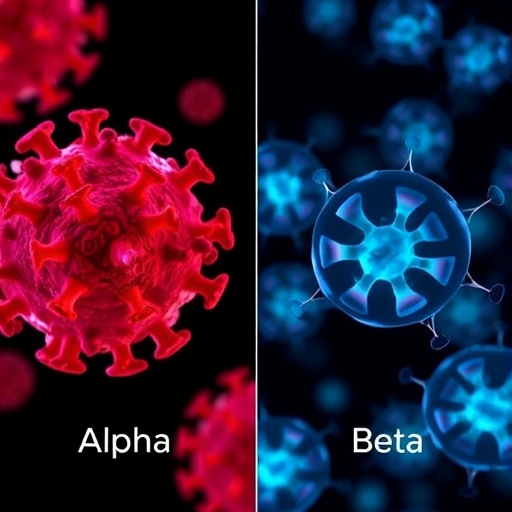
Radiopharmaceuticals have long been employed in oncology not only for their tumoricidal properties but also for their ability to modulate the tumor microenvironment. This study ventures far beyond the conventional understanding by delineating how the type of emitted radiation — alpha versus beta particles — can elicit fundamentally different immune outcomes. While both alpha and beta radiation cause localized DNA damage in cancer cells, their radiobiological impact extends into shaping the immune landscape of tumors, particularly when metastatic cancers are treated concurrently with immune checkpoint blockade.
The researchers employed murine models bearing syngeneic tumors to simulate the complex interplay between localized radiation and systemic immunotherapy. They observed that alpha-particle radiopharmaceuticals predominantly function as immune “primers.” Their high linear energy transfer (LET) deposits potent, focused energy over short distances, causing dense ionization tracks that trigger immunogenic cell death pathways remarkably efficiently. This localized destruction promotes antigen release, dendritic cell maturation, and subsequent T-cell priming in tumor-draining lymph nodes. Consequently, alpha irradiation effectively jumpstarts the adaptive immune response, setting the stage for checkpoint inhibitors to unleash a potent anti-tumor attack.
Conversely, beta-particle emitting radiopharmaceuticals exhibited a distinctive “propagating” immune effect characterized by widespread but lower intensity DNA damage. The lower LET and extended radiation path facilitate a diffused immune activation pattern across the tumor microenvironment. This spatial propagation fosters an inflamed milieu conducive to sustained T-cell infiltration and reactivation but does not induce priming with the same efficiency observed with alpha emitters. In essence, beta particles amplify existing immune responses rather than initiate them, thereby synergizing with checkpoint inhibitors in a complementary manner.
Intriguingly, combining radiopharmaceuticals with immune checkpoint inhibitors targeting PD-1 or CTLA-4 resulted in marked synergy, yet the nature of this synergy diverged sharply between alpha- and beta-particle treatments. Alpha + checkpoint blockade triggered significant expansion of naïve and memory T cell compartments, bolstering systemic immunity and yielding durable tumor regression. In contrast, the beta + checkpoint inhibitor regimen achieved tumor control primarily by sustaining effector T cell function and preventing exhaustion within the tumor bed. This dichotomy highlights the importance of mechanistic understanding in optimizing combination regimens for clinical translation.
From a molecular standpoint, the alpha radiation-induced immunogenic cell death involved enhanced calreticulin exposure, HMGB1 release, and type I interferon signaling. These hallmarks facilitated superior cross-priming of CD8+ T cells, explaining the robust systemic anti-tumor immunity observed. Beta radiation, meanwhile, augmented chemokine gradients such as CXCL9 and CXCL10, which promoted recruitment of effector T cells and myeloid populations responsible for tumor immunosurveillance and clearance. Together, these distinct immune-modulatory pathways reveal two complementary but separate therapeutic avenues.
An additional layer of complexity emerged through the assessment of tumor antigen repertoire diversity. Alpha particles enhanced the presentation of neoantigens derived from tumor mutational burden by enhancing DNA double-strand break repair errors, thereby amplifying immunogenic epitopes. Beta radiation’s effects on antigen presentation were subtler, involving upregulation of MHC class I and co-stimulatory molecules on both tumor cells and the surrounding stroma. This differential antigenic landscape modulation could inform selection of radiopharmaceutical type based on tumor genotype and immune phenotype profiling.
The ramifications of these findings are highly significant for clinical practice. Personalized cancer immunotherapy has suffered from a “one-size-fits-all” mentality regarding radiation dosing and type. This work suggests that treatment regimens should be rationally tailored: alpha emitters to prime the immune system effectively in “cold” tumors lacking pre-existing T cell infiltration, and beta emitters to propagate antitumor immunity in “hot” tumors already inflamed but requiring sustained activation. Such a paradigm shift underscores the necessity for integrated imaging and biomarker-driven patient selection.
Moreover, this study prompts reevaluation of existing clinical trials employing radiolabeled agents alongside immunotherapy. Stratifying patients not only by tumor histology and genetics but also by the physical nature of the administered radionuclide’s emissions may yield improved outcomes. The precise temporal sequencing of radiopharmaceutical administration relative to immune checkpoint inhibition also emerges as a critical variable, with alpha-based priming likely benefiting from upfront delivery prior to checkpoint blockade.
Despite the promise heralded, the translational journey from mouse models to human patients carries challenges. Patient heterogeneity in immune competence, tumor mutational landscapes, and prior therapeutic exposures must be carefully considered. Nonetheless, the mechanistic clarity provided by Kerr et al.’s work offers a robust framework for clinical trial design and biomarker discovery aimed at maximizing the therapeutic index of combined radiopharmaceutical-immunotherapy approaches.
In parallel, the safety profiles of alpha- and beta-emitting therapies differ: alpha particles’ localized high-energy deposition reduces off-target toxicity yet mandates precise targeting to avoid collateral tissue damage. Beta emitters, with their longer range, may induce bystander effects but generally provide a broader therapeutic window. Integrating these safety considerations with immune modality effects will be essential in refining dosing schedules and delivery platforms.
In conclusion, this landmark study redefines the immunological landscape of radiopharmaceuticals in cancer treatment. By distinguishing the priming capabilities of alpha particles from the propagating influences of beta particles, Kerr and colleagues illuminate a path toward precision immuno-radiotherapy. This work not only deepens our biological understanding but also empowers clinicians to strategically harness the complementary strengths of radiation physics and immune modulation. As cancer therapy continues to advance toward personalized and combinatorial regimens, such foundational insights will be instrumental in transforming patient outcomes.
The emerging concept that radiation quality governs the nature of immune engagement in tumor microenvironments opens new frontiers for biomaterial development, novel radionuclide synthesis, and immunotherapy combinations. Ultimately, this study exemplifies the power of multidisciplinary approaches bridging physics, immunology, and oncology, offering hope for improved cures in the era of immune-guided cancer therapy.
Subject of Research: Distinct immune modulatory effects of alpha- versus beta-particle emitting radiopharmaceuticals combined with immune checkpoint inhibition in cancer treatment.
Article Title: Priming versus propagating: distinct immune effects of alpha- versus beta-particle emitting radiopharmaceuticals when combined with immune checkpoint inhibition in mice.
Article References:
Kerr, C.P., Jin, W.J., Liu, P. et al. Priming versus propagating: distinct immune effects of alpha- versus beta-particle emitting radiopharmaceuticals when combined with immune checkpoint inhibition in mice.
Nat Commun (2026). https://doi.org/10.1038/s41467-026-68834-1
Image Credits: AI Generated
Tags: alpha-particle radiopharmaceuticalsbeta-particle radiopharmaceuticalscancer immunotherapy advancementsimmune checkpoint inhibitorsimmune landscape shapingimmune responses in oncologylocalized DNA damage in cancermetastatic cancer treatment strategiesradiobiological impact of radiationsyngeneic tumor modelstherapeutic strategies against resistant tumorstumor microenvironment modulation