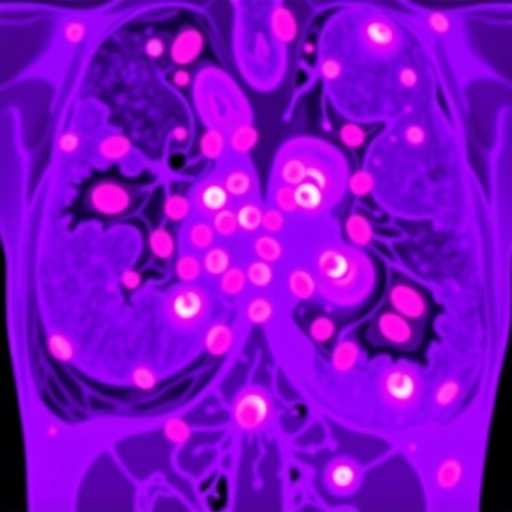
In recent years, the intersection of artificial intelligence and oncology has yielded groundbreaking insights into the complex dynamics of tumor microenvironments. A notable study by Xie, Ai, and Liu et al., published in the Journal of Translational Medicine, investigates two distinct immune subtypes characterized by tumor-infiltrating lymphocytes (TILs) in the context of triple-negative breast cancer (TNBC). This exploration of focal hotspot and diffuse immune subtypes provides a rich understanding of their clinical relevance, particularly concerning HER2 expression, a crucial biomarker in breast cancer management. With the power of AI-driven spatial clustering techniques, this research not only sheds light on the intricate immune landscape of tumors but also offers promising avenues for personalized medicine, aiming to enhance therapeutic outcomes for patients.
Artificial intelligence has become an invaluable tool in various scientific disciplines, particularly in the analysis and interpretation of complex biological data. In oncology, AI algorithms can analyze vast amounts of spatial data to unveil patterns that might elude traditional methods. The study by Xie and colleagues employs these advanced computational techniques to classify tumor-infiltrating lymphocytes based on their spatial distribution within tumor tissues. By delineating focal hotspots from diffuse immune patterns, the researchers can conclude how these distributions correlate with HER2 expression and tumor aggressiveness.
In triple-negative breast cancer, the absence of estrogen receptors, progesterone receptors, and HER2 overexpression presents a unique challenge. This subtype of breast cancer is often associated with a poorer prognosis and a lack of targeted therapies. Consequently, understanding the dual landscape of TILs could unravel correlations between immune responses and therapeutic resistance. The researchers meticulously categorized TILs, emphasizing their role in anti-tumor immunity and their potential contribution to treatment responses.
The classification of TILs into focal hotspots and diffuse immune patterns poses critical implications for clinical practice. Focal hotspots may indicate areas of intense immune activity, potentially correlating with better responses to immunotherapy. In contrast, diffuse patterns might signal areas where tumors evade immune surveillance, suggesting a need for more aggressive therapeutic strategies. This duality highlights that not all TILs operate under a uniform mechanism; instead, their spatial distribution can dictate their functional capabilities and, ultimately, their influence on patient outcomes.
A significant aspect of this research lies in its integration of HER2 expression levels with immune landscape characterization. HER2 is a well-established driver of tumor growth in a subset of breast cancers, yet its relationship with immune cell infiltration remains complex and often contradictory. The AI-powered spatial clustering analysis employed in this study uncovers nuances in how HER2 expression might modulate immune responses. For instance, tumors with high HER2 expression could exhibit a different TIL pattern compared to those lacking HER2 amplification, which might influence treatment decisions.
Furthermore, the implications of these findings extend beyond mere classification. By correlating TIL subtypes with HER2 expression and other clinical parameters, the study opens doors to stratifying patients based on their immune landscape. This stratification could enable a more tailored approach to therapy, potentially directing patients towards immunotherapeutic options or HER2-targeted treatments, depending on their unique tumor immune interactions.
The innovative approach of employing AI for spatial analysis is another noteworthy feature of this research. Traditional methods of assessing immune cell distribution often rely on manual counts of cell densities, which can be both tedious and prone to human error. The application of AI-driven algorithms, however, allows for rapid and accurate assessments of TIL distributions, providing a robust framework for classifying tumor microenvironments. This adaptability not only streamlines the analytical process but also enhances reproducibility and scientific rigor.
This study also invites further questions regarding the heterogeneity of the immune landscape. The identification of focal hotspots and diffuse subtypes suggests a need for deeper explorations into the molecular mechanisms driving these patterns. Future research could delve into the signaling pathways that govern TIL behavior within these distinct regions, potentially illuminating new therapeutic targets. Understanding these mechanisms will be crucial for translating these findings into clinical practice, particularly in optimizing immunotherapy approaches in TNBC.
Moreover, as the field advances, the integration of multi-omics approaches alongside AI models will likely yield even more nuanced insights into tumor immunity. By combining genomic, transcriptomic, and proteomic data with spatial analyses of immune cell distributions, researchers can construct a more comprehensive view of the tumor immune microenvironment. This holistic perspective could facilitate the identification of biomarkers predictive of treatment responses, enhancing the precision of therapeutic interventions.
In sum, the research by Xie, Ai, and Liu et al. marks a significant milestone in the exploration of immune landscape dynamics in triple-negative breast cancer. By dissecting TIL spatial distributions and their relationship with HER2 expression, this study has profound implications for understanding tumor immunity and shaping future treatment paradigms. The promising intersection of AI and oncology heralds a new era of personalized medicine, where therapies can be tailored to individual tumor characteristics, ultimately leading to more effective patient management.
As the dialogue around the immune landscape of tumors continues to evolve, studies like this one underscore the urgent need for integrating advanced technologies into cancer research. The success of AI in elucidating complex biological phenomena not only heralds a transformation in our understanding of cancer biology but also brings us closer to achieving the ultimate goal of personalized therapeutic strategies. The passage from basic research findings to clinical application is often lengthy, yet the potential breakthroughs such as those revealed in Xie et al.’s work are paving the way for a more nuanced understanding of cancer treatment.
Amidst the backdrop of evolving treatment paradigms in breast cancer, the role of immune modulation is increasingly recognized as a cornerstone strategy. As researchers continue to unveil the complex interactions between tumor cells and immune components, we anticipate a future where personalized immunotherapy becomes a mainstay of treatment regimens. Ultimately, fostering a collaborative effort between computational biology and clinical oncology will empower us to face the challenges posed by aggressive malignancies like triple-negative breast cancer head-on.
Moving ahead, it’s clear that the intersection of artificial intelligence and oncology is not merely an academic curiosity but rather a driving force shaping the future of therapeutic strategies. The ongoing studies that explore the multifaceted interactions within tumor microenvironments will undoubtedly pave the way for innovative diagnostic and treatment modalities, finally actualizing the promise of precision medicine in oncology.
Subject of Research: Tumor-infiltrating lymphocytes in triple-negative breast cancer
Article Title: Focal hotspot and diffuse immune subtypes of tumor-infiltrating lymphocytes: AI-powered spatial clustering classification and its clinical relevance to HER2 expression in triple-negative breast cancer
Article References:
Xie, T., Ai, S., Liu, C. et al. Focal hotspot and diffuse immune subtypes of tumor-infiltrating lymphocytes: AI-powered spatial clustering classification and its clinical relevance to HER2 expression in triple-negative breast cancer.
J Transl Med (2025). https://doi.org/10.1186/s12967-025-07608-7
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07608-7
Keywords: triple-negative breast cancer, tumor-infiltrating lymphocytes, HER2 expression, artificial intelligence, spatial clustering, immune microenvironment.
Tags: AI in OncologyAI-driven spatial clustering techniquesbreast cancer researchcomputational analysis of biological dataHER2 expression in breast cancerimmune landscape of tumorsimmune subtypes in cancerpersonalized medicine in oncologytherapeutic outcomes in breast cancer patientstriple-negative breast cancer insightstumor microenvironment dynamicstumor-infiltrating lymphocytes classification