Recent advancements in the realm of immunology have paved pathways toward understanding the complexities of autoimmune diseases. A groundbreaking study conducted by Wang et al. has illuminated previously unexplored aspects of autoimmune pancreatitis, particularly focusing on the age-associated B cells (ABCs) present in the pancreas. Utilizing cutting-edge single-cell multi-omics analysis techniques, this research provides deep insights into how the immune system adapts and responds in the context of type 1 autoimmune pancreatitis.
Autoimmune pancreatitis is a highly intricate condition marked by the body’s immune system mistakenly targeting its own pancreatic tissues. This aberrant immune response manifests in chronic inflammation and can lead to significant clinical outcomes, encompassing pain, weight loss, and complications related to impaired pancreatic function. Understanding the cellular dynamics in this disease is paramount for developing targeted therapies and improving patient outcomes.
The innovative methodology employed by Wang and his colleagues involved single-cell multi-omics analysis. This sophisticated technique integrates genomic, transcriptomic, and proteomic data, enabling a comprehensive evaluation of individual cell behaviors and interactions. Such an in-depth analysis is particularly vital for elucidating how different immune cell populations, including B cells, contribute to the pathology of autoimmune pancreatitis.
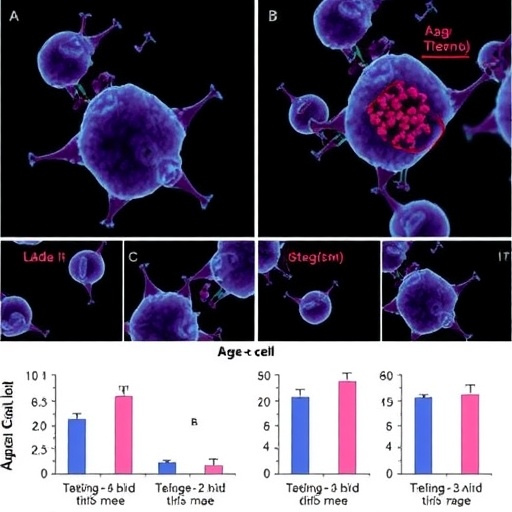
B cells, a central component of the adaptive immune system, are responsible for antibody production. In the context of autoimmune diseases, dysregulation or aberrant expansion of specific B cell populations can exacerbate the disease process. Wang et al.’s study highlights a notable expansion of age-associated B cells (ABCs) within the pancreatic microenvironment of patients with type 1 autoimmune pancreatitis. This finding emphasizes the potential role that aging and immune system changes play in the pathogenesis of autoimmune diseases.
The expansion of ABCs suggests a shift in the immune profile of pancreatic tissues over time, indicating that age may influence the development of autoimmune pancreatitis. This aspect of the research raises intriguing questions about the interaction between aging and immune response, particularly how physiological changes associated with aging can predispose individuals to autoimmune conditions.
Understanding the age-associated B cell population opens up new avenues for therapeutic strategies. If ABCs are found to contribute significantly to the autoimmune response, targeting these cells could potentially halt or reverse the progression of the disease. Wang and his team’s study not only identifies these B cells but also suggests mechanisms through which they may exacerbate inflammation and tissue damage in autoimmune pancreatitis.
Additionally, the implications of this research extend beyond just autoimmune pancreatitis. The findings may have broader relevance for understanding other autoimmune diseases where age-related immune changes play a role. Recognizing that the immune landscape evolves with age can inform approaches for therapeutic interventions in various conditions characterized by immune dysregulation.
The detailed exploration of the pancreatic microenvironment conducted in this study also sheds light on the intricate interplay between various immune cells and their local environment. It underscores the significance of microenvironmental factors in shaping immune responses, which could guide future research in immunotherapy. By unraveling the complexities found in the pancreas of autoimmune pancreatitis patients, further investigations may yield pivotal insights applicable not only in pancreatic diseases but also across the broader field of immunology.
Moreover, Wang et al.’s research reinforces the importance of single-cell technologies in modern biomedical research. The ability to dissect cellular populations at an unprecedented resolution allows for the identification of specific cell types and states that are overlooked in bulk analyses. This has revolutionized our understanding of disease mechanisms and offers a promising framework for precision medicine.
As the field of immunology progresses, studies like this serve as vital stepping stones toward novel therapeutic strategies and a more nuanced understanding of autoimmune diseases. It emphasizes the necessity of integrating genomic analysis with clinical observations to unveil critical aspects of the immune system’s behavior over time.
In conclusion, Wang et al.’s research is set to redefine our comprehension of age-related changes in immune responses, especially in the context of autoimmune pancreatitis. Their findings illustrate the unique characteristics of age-associated B cells and prompt further inquiries into targeted therapeutic strategies, presenting a beacon of hope for patients enduring this challenging condition.
This evolving narrative in autoimmune research is not just about understanding pathophysiology; it is about transforming how we approach treatment and management of diseases that afflict millions worldwide. The prospect of leveraging single-cell analysis to refine our understanding of immune responses heralds a new era where personal and age-specific therapies may soon be a reality.
Currently, as the data suggests a profound connection between age, immune system dynamics, and autoimmune pathology, the scientific community stands on the brink of significant change. The ongoing dialogue generated by these findings underscores the critical need for collaborative research, aiming to bridge gaps in knowledge and fast-track innovative treatment modalities tailored to individual needs.
The journey of discovery continues, driven by the remarkable potential of scientific inquiry to transform lives. As Wang et al. showcase, the future of immunological research is bright, filled with the promise of breakthroughs that could one day translate into effective interventions for those at risk of or suffering from autoimmune diseases across the spectrum.
Through relentless exploration and technological advancement, we inch closer to a comprehensive understanding of our immune landscape, ultimately fostering hope for improved patient outcomes and a deeper appreciation of the human body’s resilience.
Subject of Research: Autoimmune pancreatitis and age-associated B cells
Article Title: Single-cell multi-omics analysis revealed the expansion of age-associated B cells in the pancreas of type 1 autoimmune pancreatitis patients.
Article References:
Wang, J., Liu, C., Zhang, X. et al. Single-cell multi-omics analysis revealed the expansion of age-associated B cells in the pancreas of type 1 autoimmune pancreatitis patients.
Genome Med 17, 138 (2025). https://doi.org/10.1186/s13073-025-01567-w
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13073-025-01567-w
Keywords: Autoimmune disease, pancreatic inflammation, single-cell analysis, B cells, age-associated immune response, multi-omics.
Tags: adaptive immune system and B-cellsage-related B cell expansionautoimmune disease immunologyB cell dynamics in autoimmune conditionscellular interactions in pancreatic diseaseschronic inflammation in autoimmune pancreatitisimplications of age on immune functionpancreatic immune responsesingle-cell multi-omics analysistargeted therapies for pancreatitistype 1 autoimmune pancreatitisunderstanding autoimmune pancreatitis pathology