In recent years, sarcopenia has emerged from the shadows of geriatric medicine to claim attention within younger demographics, ushering in a new era of research that challenges longstanding perceptions. Traditionally viewed as an inevitable consequence of aging or chronic debilitating diseases, sarcopenia—the progressive decline of muscle mass and strength—now demands recognition within the pediatric population. This expanding paradigm shift opens a critical dialogue on the early onset of muscle deterioration among children and adolescents, suggesting that muscle health interventions must commence far earlier than previously assumed.
The conventional understanding of sarcopenia has been anchored in its association with aging, typically diagnosed via diminished muscle quantity and functional capacity in the elderly. However, recent investigations expose a striking prevalence of muscle deficits in pediatric groups, with estimates indicating that nearly 30% of adolescents may experience some degree of sarcopenia. This discovery provokes an urgent need for the scientific community to develop robust diagnostic frameworks tailored to pediatric physiology. Without these specialized criteria, early identification and timely intervention remain elusive, enhancing vulnerability to adverse metabolic conditions and chronic non-communicable diseases later in life.
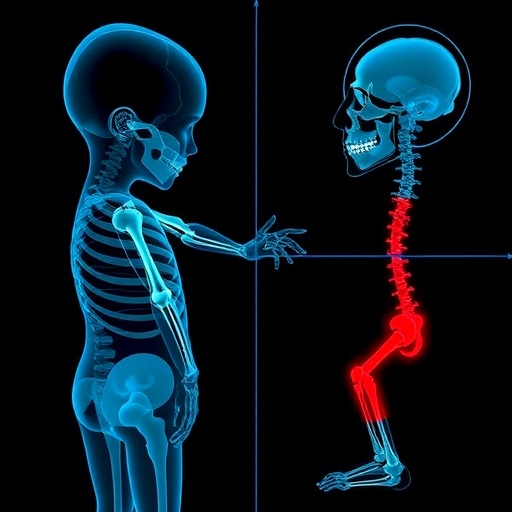
Muscle health in children is complex, influenced by a dynamic interplay of genetic, nutritional, physical, and environmental factors. The emerging concept of the muscle mass-strength-functionality triad (MSFt) offers a comprehensive lens through which pediatric sarcopenia can be assessed. Unlike previous approaches focused exclusively on muscle mass or isolated strength measurements, the MSFt integrates three critical dimensions: muscle quantity, contractile strength, and physical performance capacity. This triadic relationship is pivotal for a holistic understanding of how muscular deficits impair daily functionality and long-term health trajectories in young populations.
Incorporating the MSFt into pediatric diagnostics represents a paradigm shift from reductionist evaluations to a multifaceted perspective on muscle health. This approach allows clinicians and researchers to decipher the nuances of muscle development disruption, distinguishing between mere quantitative muscle loss and functional inefficiencies that can coexist or exist independently. For instance, two children with equivalent muscle mass may exhibit vastly different strength profiles or physical capabilities, underscoring the necessity of multidimensional assessment tools.
The deficit of standardized criteria for diagnosing pediatric sarcopenia has posed significant hurdles to research and clinical implementation. Unlike the adult population, for which consensus definitions such as those from the European Working Group on Sarcopenia in Older People (EWGSOP) exist, pediatric guidelines remain embryonic. The heterogeneity of growth rates, pubertal status, and physical maturation further complicates defining normative thresholds, necessitating large, diverse cohorts to establish age- and sex-specific reference values that reliably delineate physiological muscle development from pathological decline.
Recent cohort studies employing dual-energy X-ray absorptiometry (DXA), bioelectrical impedance analysis (BIA), and handgrip dynamometry have begun to map these normative values for muscle mass and strength in children. Yet, a significant gap remains in accessing functional performance metrics that reflect real-world physical abilities, such as gait speed or timed up-and-go tests, which are critical in adult sarcopenia diagnosis. Advances in wearable technology and motion capture systems promise to bridge this gap by providing objective, high-resolution data on pediatric muscle functionality in everyday settings.
Beyond the technical diagnostic challenges, an underappreciated factor influencing pediatric muscle health is the concept of physical literacy. Defined as the motivation, confidence, physical competence, knowledge, and understanding to value and engage in physical activities, physical literacy lays the foundation for lifelong health and wellness. Deficits in fundamental movement skills during childhood may predispose to decreased physical activity levels, accelerating muscle atrophy and functional decline. Thus, promoting physical literacy within school curricula and community programs emerges as a critical preventive strategy against pediatric sarcopenia.
The pathophysiological implications of early-onset sarcopenia extend far beyond muscle mass loss. Children affected by diminished muscle strength and function face increased susceptibility to insulin resistance, adiposity, and dyslipidemia, components of metabolic syndrome that can catalyze the onset of type 2 diabetes and cardiovascular diseases. These metabolic disturbances intertwine with chronic non-communicable diseases, creating a cascading effect that compromises overall pediatric health and escalates healthcare burdens on a societal level.
Mechanistically, sarcopenia involves alterations in muscle fiber composition, reduced satellite cell activity, impaired neuromuscular junction functionality, and chronic low-grade inflammation—processes all susceptible to modulation by lifestyle factors in childhood. Understanding these intrinsic and extrinsic contributors to muscle decline is essential for developing targeted therapeutic interventions, including nutritional supplementation, resistance training regimens, and pharmacological agents aimed at preserving or restoring muscle integrity in youthful populations.
The integration of novel biomarkers also holds promise in refining pediatric sarcopenia diagnostics. Circulating factors such as myostatin, inflammatory cytokines, and muscle-specific microRNAs may serve as early indicators of muscle deterioration before overt clinical manifestations. Future research capitalizing on omics technologies and machine learning algorithms could yield predictive models that facilitate personalized risk assessments, enabling preemptive measures for children identified as high risk for sarcopenia-related complications.
There is a robust call within the scientific community to harmonize efforts toward establishing an international consensus on pediatric sarcopenia. Collaborative initiatives spanning epidemiology, physiology, pediatrics, and rehabilitation sciences are paramount for pooling data, validating assessment tools, and clarifying terminology. Such global synergy will accelerate the development of evidence-based clinical guidelines that safeguard muscle health from infancy through adolescence.
Intervention strategies must parallel diagnostic advancements; emphasis should be placed on interventions that holistically target the MSFt components. Structured physical activity programs enriched with resistance and functional training, alongside nutritional interventions optimizing protein intake and micronutrient status, should be implemented within pediatric healthcare protocols. Importantly, interventions must be age-appropriate, culturally sensitive, and designed to engage families and caregivers for sustained adherence and efficacy.
As research progresses, the psychosocial aspects of pediatric sarcopenia warrant attention. Muscle weakness and physical limitations can negatively impact self-esteem, social integration, and mental health in children. Integrative approaches that combine physical rehabilitation with psychological support can enhance overall outcomes, underscoring muscle health as a multidimensional domain involving both physical and emotional well-being.
Current gaps notwithstanding, the emerging evidence underscores the imperative to view sarcopenia not solely as an aging-related syndrome but as a lifelong condition whose roots extend into early development stages. This reconceptualization challenges healthcare providers, researchers, and policymakers to redefine pediatric muscle health priorities and allocate resources accordingly toward surveillance, prevention, and treatment efforts.
In conclusion, advancing the diagnosis of sarcopenia in children necessitates a holistic understanding of muscle mass, strength, and functional capacity as interdependent factors. The muscle mass-strength-functionality triad (MSFt) embodies this integrative approach, providing a conceptual and operational framework to guide future research and clinical practice. Coupled with initiatives to improve physical literacy and fundamental movement skills, such efforts promise to mitigate the burgeoning pediatric sarcopenia burden, paving the way for healthier, more active generations.
The evolution of sarcopenia research marks a transformative moment in pediatric medicine, bridging gaps between muscle biology, functional capacity, and public health. As studies continue to unravel the complexities of early muscle decline, the path toward standardized diagnostic criteria and effective interventions becomes clearer. Embracing this challenge will ensure that children at risk receive timely care and the opportunity to achieve their full muscular potential long before the specter of age-related decline looms.
Subject of Research: Pediatric sarcopenia; muscle mass, strength, and functionality interplay; development of diagnostic criteria for early muscle health decline in children and adolescents.
Article Title: Perspective Review: Advancing toward the diagnosis of sarcopenia in the pediatric population.
Article References:
Flores-Opazo, M., Monsalves-Álvarez, M., Sepúlveda-Guzmán, C. et al. Perspective Review: Advancing toward the diagnosis of sarcopenia in the pediatric population. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04716-4
Image Credits: AI Generated
DOI: 26 December 2025
Tags: chronic diseases in childrendiagnostic frameworks for pediatric sarcopeniaearly onset muscle deteriorationenhancing muscle strength in youthgenetic influences on muscle healthintervention strategies for sarcopeniamuscle health in childrennutritional factors in pediatric sarcopeniapediatric muscle mass declinepediatric sarcopenia diagnosissarcopenia in adolescentsunderstanding pediatric muscle deficits