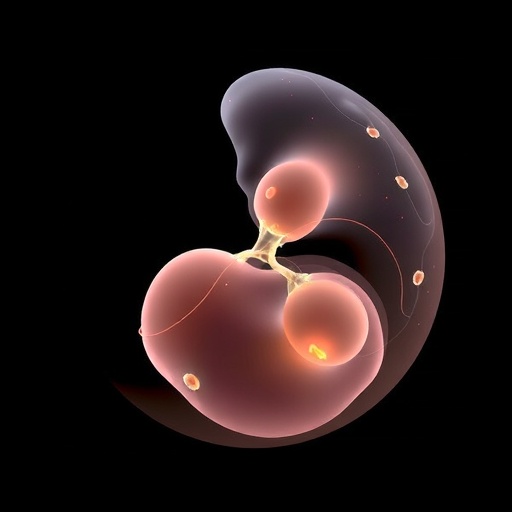
In recent years, the convergence of artificial intelligence (AI) with medical science has sparked significant advancements, particularly in the realm of reproductive health. With the increasing prevalence of assisted reproductive technologies (ART), the need for refined methodologies to improve embryo grading and predict pregnancy outcomes has become paramount. A groundbreaking review by Ouyang and Wei unveils the potential of multi-modal artificial intelligence systems in revolutionizing these processes, providing insights essential for both practitioners and patients navigating the often complex ART landscape.
The development of multi-modal AI refers to systems that integrate data from various sources to enhance decision-making processes. In the context of embryo grading, this approach combines image analysis, genomic data, and clinical histories, thus enabling a comprehensive and nuanced evaluation of embryos. By utilizing algorithms that can analyze visual features alongside genetic markers, these AI models show promise in identifying the highest quality embryos for transfer during in vitro fertilization (IVF), ultimately aiming to improve pregnancy rates while minimizing the risk of multiple gestations.
Traditionally, embryo grading has relied heavily on the expertise of embryologists who assess embryos based on a limited set of parameters. This subjective methodology can lead to variability in evaluation, resulting in inconsistent outcomes for patients. However, AI’s ability to process vast amounts of data at rapid speeds presents a unique opportunity to standardize grading procedures. The review highlights various studies where AI systems demonstrated superior accuracy compared to human assessments, underscoring the potential such technology holds to enhance the reliability of embryo selection.
The integration of multi-modal AI doesn’t end at embryo grading; it also extends to predicting pregnancy outcomes post-transfer. The ability to analyze diverse datasets—such as hormonal profiles, patient age, and lifestyle factors—allows AI to construct predictive models that can provide individualized risk assessments. By identifying patterns associated with successful or unsuccessful pregnancies, these systems can help clinicians customize treatment plans more effectively, thus enhancing patient experiences and outcomes during ART procedures.
Moreover, as the authors Ouyang and Wei elucidate, the synergy between AI and genomic data can transform the landscape of reproductive health. Genomic screening of embryos, for instance, improves the understanding of genetic anomalies that may interfere with development. When combined with AI’s analytical capabilities, this information can lead to more informed decisions by embryologists, potentially increasing the likelihood of a successful pregnancy. Such integration not only enhances clinical decision-making but may also alleviate some ethical concerns associated with genetic testing in reproductive medicine.
However, the integration of AI into clinical settings is not devoid of challenges. The authors cautiously discuss the hurdles of data privacy, algorithm transparency, and the necessity for stringent validation studies. As AI systems become more prevalent, it is crucial that they are accompanied by rigorous regulatory frameworks to ensure both safety and efficacy. Transparency in how these models derive their recommendations is particularly vital to gaining trust from both practitioners and patients, as the hesitancy towards AI adoption often stems from fears of the unknown.
The results from various case studies mentioned in the review are promising. One noteworthy study referenced demonstrates how a multi-modal AI system achieved a remarkable 90% accuracy in predicting implantation success rates based on a combination of embryo characteristics and maternal health data. Such findings advocate for the indispensable role that AI could play in shaping future ART practices. They offer a beacon of hope for individuals and couples struggling with infertility, perhaps leading to innovative solutions and increased success rates in achieving pregnancy.
As the discourse around the use of AI in medicine unfolds, educational initiatives targeting both healthcare providers and patients are crucial. Building an understanding of AI’s capabilities, potential, and limitations can help foster more positive attitudes toward its incorporation in clinical routines. The authors emphasize the need for training programs that familiarize professionals with AI tools, thus preparing them to leverage these technologies effectively in their practices.
Furthermore, the implications of incorporating AI into ART extend beyond clinical outcomes. By improving success rates, AI technology could also have significant economic impacts within the healthcare system. Fewer unsuccessful IVF attempts could lead to reduced costs for both patients and clinics, thereby increasing accessibility to ART services. As such, the economic benefits associated with AI integration into embryo grading and pregnancy prediction is an avenue that invites further exploration.
In conclusion, the insights presented by Ouyang and Wei encapsulate the transformative potential of multi-modal artificial intelligence in assisted reproductive technology. The journey toward integrating AI systems into routine clinical practice, however, requires a balanced approach that weighs both innovation and the ethical considerations that accompany such advancements. As the field of reproductive medicine continues to evolve, it is anticipated that these intelligent systems will pave the way for more successful interventions, ultimately fostering hope for countless individuals aspiring to start or expand their families.
As research in this domain progresses, continuous evaluations of AI’s impact will be crucial. With ongoing collaborations between engineers, data scientists, and reproductive specialists, the insights derived from AI will remain critical in navigating the complexities of ART. The ambition of achieving higher success rates and improved patient care remains at the forefront, and the evolution of AI in this sector promises to bring significant breakthroughs that benefit reproductive health in the years to come.
Subject of Research: Multi-modal Artificial Intelligence in Embryo Grading and Pregnancy Prediction
Article Title: Multi-modal Artificial Intelligence of Embryo Grading and Pregnancy Prediction in Assisted Reproductive Technology: A Review
Article References:
Ouyang, X., Wei, J. Multi-modal Artificial Intelligence of Embryo Grading and Pregnancy Prediction in Assisted Reproductive Technology: A Review.
Ann Biomed Eng (2025). https://doi.org/10.1007/s10439-025-03865-1
Image Credits: AI Generated
DOI: 10.1007/s10439-025-03865-1
Keywords: Artificial Intelligence, Embryo Grading, Pregnancy Prediction, Assisted Reproductive Technology, In Vitro Fertilization, Genomic Data, Clinical Outcomes
Tags: AI algorithms for embryo quality assessmentAI in reproductive healthassisted reproductive technologies advancementschallenges in traditional embryo gradingdecision-making in reproductive medicineembryo evaluation using image analysisenhancing embryo transfer success ratesgenomic data in IVF processesimproving pregnancy prediction with AIintegrating clinical histories in reproductive health AI.minimizing risks in multiple gestationsmulti-modal artificial intelligence in embryo grading