A recent case report published in Cyborg Bionic Systems details the diagnosis of Idiopathic Normal Pressure Hydrocephalus (iNPH) using multimodality diagnostic approaches, highlighting significant advancements in medical diagnostics and patient care. The study conducted by a team of researchers from Tianjin Medical University General Hospital, Tianjin, China, presents a comprehensive case study of a 68-year-old male patient diagnosed with iNPH, showcasing the effectiveness of these advanced diagnostic techniques.
A recent case report published in Cyborg Bionic Systems details the diagnosis of Idiopathic Normal Pressure Hydrocephalus (iNPH) using multimodality diagnostic approaches, highlighting significant advancements in medical diagnostics and patient care. The study conducted by a team of researchers from Tianjin Medical University General Hospital, Tianjin, China, presents a comprehensive case study of a 68-year-old male patient diagnosed with iNPH, showcasing the effectiveness of these advanced diagnostic techniques.
iNPH is a condition characterized by the accumulation of cerebrospinal fluid (CSF) causing ventricular dilation, often mistaken for brain atrophy due to similar symptoms such as cognitive impairment and gait disturbances. The prevalence of this condition increases with age, affecting approximately 1.30% of individuals over 65 and rising to 5.9% among those over 80.
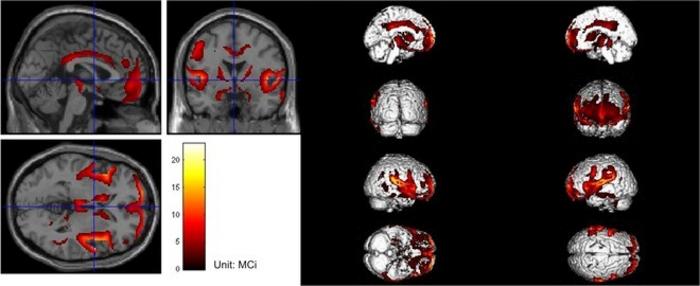
In the documented case, the patient suffered from deteriorated gait, cognitive decline, and urinary incontinence, symptoms that gradually worsened over several years. Initially misdiagnosed, his condition prompted the use of multimodality diagnostic approaches after traditional methods provided inconclusive results. The diagnostic process included brain imaging, cerebrospinal fluid tap tests (CSFTT), continuous intracranial pressure monitoring, and a novel infusion study, which collectively led to an accurate diagnosis and subsequent treatment.
The infusion study, a critical component of the diagnosis, involves the measurement of cerebrospinal fluid resistance (Rcsf), which has been identified as a crucial physical marker for diagnosing hydrocephalus. In this case, an Rcsf level exceeding the normal range significantly indicated the presence of hydrocephalus, confirming the necessity for surgical intervention.
Following the diagnosis, the patient underwent a ventriculoperitoneal shunt surgery, which involves the insertion of a tube to drain excess CSF from the brain to the abdominal cavity. The surgery was successful, with the patient showing remarkable improvement in symptoms and overall quality of life.
This case underscores the vital role of multimodality diagnostic approaches in the medical field. Not only do these techniques enhance diagnostic accuracy, but they also reduce clinical costs and time spent in diagnosis, providing a quicker path to recovery for patients. The effectiveness of these approaches in complex cases like iNPH demonstrates their potential for broader application, promising significant improvements in the diagnosis and treatment of similar conditions.
Moreover, the study advocates for the adoption of these techniques in standard medical practice, suggesting that they could significantly reduce the rates of misdiagnosis and improve clinical outcomes. As medical technology continues to advance, the integration of such multimodal diagnostic tools holds the promise of transforming patient care, offering more precise, efficient, and cost-effective solutions for challenging medical diagnoses.
The paper, “A Male Patient with Hydrocephalus via Multimodality Diagnostic Approaches: A Case Report” was published in the journal Cyborg and Bionic Systems on Jul 1, 2024, at DOI: https://spj.science.org/doi/10.34133/cbsystems.0135
Journal
Cyborg and Bionic Systems
DOI
10.34133/cbsystems.0135