A person’s genetic makeup plays a role in autoimmune diseases such as multiple sclerosis that develop when the body is attacked by its own immune system. But little is known about how immune cells are pushed into overdrive.
Now, in new research that points to potential therapeutic targets for autoimmune diseases, researchers at Washington University School of Medicine in St. Louis have identified genetic master switches that turn up – or down – the activity of specific types of immune cells.
Surprisingly, the regions of DNA that make up these master switches include numerous genetic variants linked to a range of autoimmune diseases, the researchers found.
The study is available online in Cell.
“These regions of DNA typically act like master dimmer switches on the activity of these immune cells,” said Eugene Oltz, PhD, a professor of pathology and immunology at Washington University and co-senior author on the study. “In some cases, individual variations in a person’s DNA probably tweak the settings of these switches upward, leading to overactivation of the immune cells and autoimmune disease.”
Oltz and co-senior author Marco Colonna, MD, the Robert Rock Belliveau, MD, Professor of Pathology at Washington University, did not originally set out to link genetic variants associated with autoimmune diseases to these switches in immune cells. They were trying to understand how two different types of immune cells could play the same role in fighting pathogens.
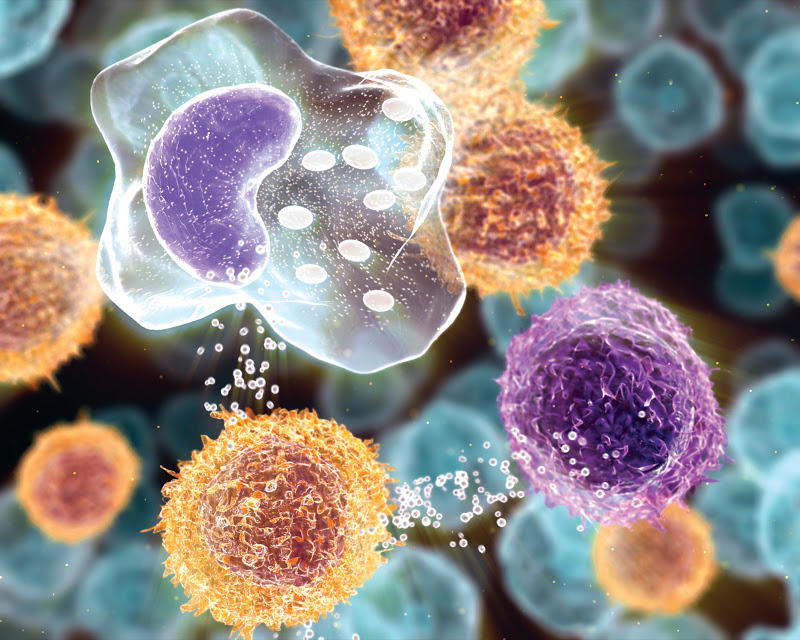
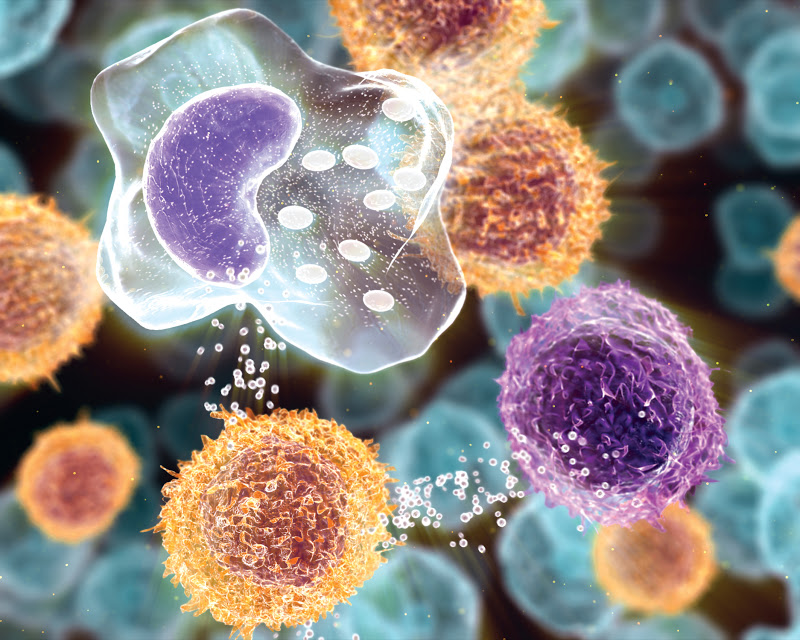
Specifically, innate lymphoid cells act quickly when a pathogen invades the body, responding to non-specific danger signals released by the cells at the site of infection. In contrast, T helper cells take days to respond, and only activate when they encounter a pathogen they recognize.
Despite being activated at different times and by different signals, innate lymphoid cells and T helper cells both serve as a kind of control tower for the immune response, sending out powerful molecular signals to other immune cells to unsheathe their weapons and start killing invading microbes and destroying infected human cells.
If the signals are not tightly controlled, these weapons can be turned on human cells, resulting in chronic inflammation and the development of autoimmune conditions.
“How is it possible that innate lymphoid cells and T helper cells produce the same signaling molecules in response to invading pathogens despite being activated by different signals?” Colonna asked. “We started to look at the similarities and differences in the way gene expression in these two cell types was regulated.”
Using cells from human tonsils, the researchers compared the patterns of gene activity in the two types of cells. They were able to define a set of super-enhancers – regions of DNA that serve as master control switches – for innate lymphoid cells and T helper cells that regulate genes which give each cell type its unique identity and function.
“This is the first time that these sets of super-enhancers had been mapped for these cell types,” Oltz said. “By looking at these super-enhancers, we were able to identify a number of genes that are likely to be critical for eliminating pathogens, but which nobody had identified as important before.”
Furthermore, the researchers found that the super-enhancers contained many genetic variants associated with autoimmune diseases such as diabetes, rheumatoid arthritis, Crohn’s disease and ulcerative colitis. This observation could pave the way to more personalized treatments for autoimmune diseases, the researchers said. For example, patients could be divided into groups based on the super-enhancer in which their genetic variant falls, and therapies could be targeted to the genes regulated by each specific super-enhancer.
“Geneticists have identified lots of DNA sequence variations associated with autoimmune diseases, but it wasn’t clear how they were involved because they weren’t in any genes known to be involved in the development of these diseases,” Colonna said. “We are the first ones to locate the variations in the landscape of innate lymphoid cell regulation. Now that we know where the master switches are, we can see that those variants are associated with autoimmune disease because they affect the regulation of these immune cells.”
###
Media Contact
Tamara Bhandari
[email protected]
314-286-0122
@WUSTLmed
Home
The post New clues found to immune system’s misfiring in autoimmune diseases appeared first on Scienmag.