Credit: Paul Titchenell, PhD, Perelman School of Medicine, University of Pennsylvania
PHILADELPHIA — A new animal study shows how insulin controls the movement and storage of fat molecules in the liver and how a breakdown in this system could lead to non-alcoholic fatty liver disease and changes in circulating lipid levels associated with cardiovascular disease. Researchers from the Perelman School of Medicine at the University of Pennsylvania published their findings this week in the Journal of Clinical Investigation (JCI).
"The production of triglyceride in the liver and its secretion into blood are closely linked to nutrient availability and insulin levels," said senior author Paul Titchenell, PhD, an assistant professor of Physiology and a member of the Institute for Diabetes, Obesity, and Metabolism. "After a meal, insulin tells the liver to package and secrete excess nutrients into triglyceride-rich lipid particles into the blood for use by the rest of the body."
After eating, glucose rises, which induces insulin release to control blood sugar levels by increasing glucose uptake and reducing glucose production by the liver. In addition to glucose regulation, insulin also controls blood lipid levels in part by increasing lipid synthesis, uptake, and storage in fat cells.
In the JCI paper, the team demonstrated that mTOR complex 1 (mTORC1), a protein super-molecule made up of several smaller proteins, is essential for very low density lipoprotein (VLDL)-triglyceride production. VLDL-triglyceride molecules are exported by the liver and carry lipids to peripheral tissues. "This is important because in metabolic diseases associated with insulin resistance the liver makes more triglycerides, which leads to increased levels in the blood and eventually cardiovascular disease," Titchenell said.
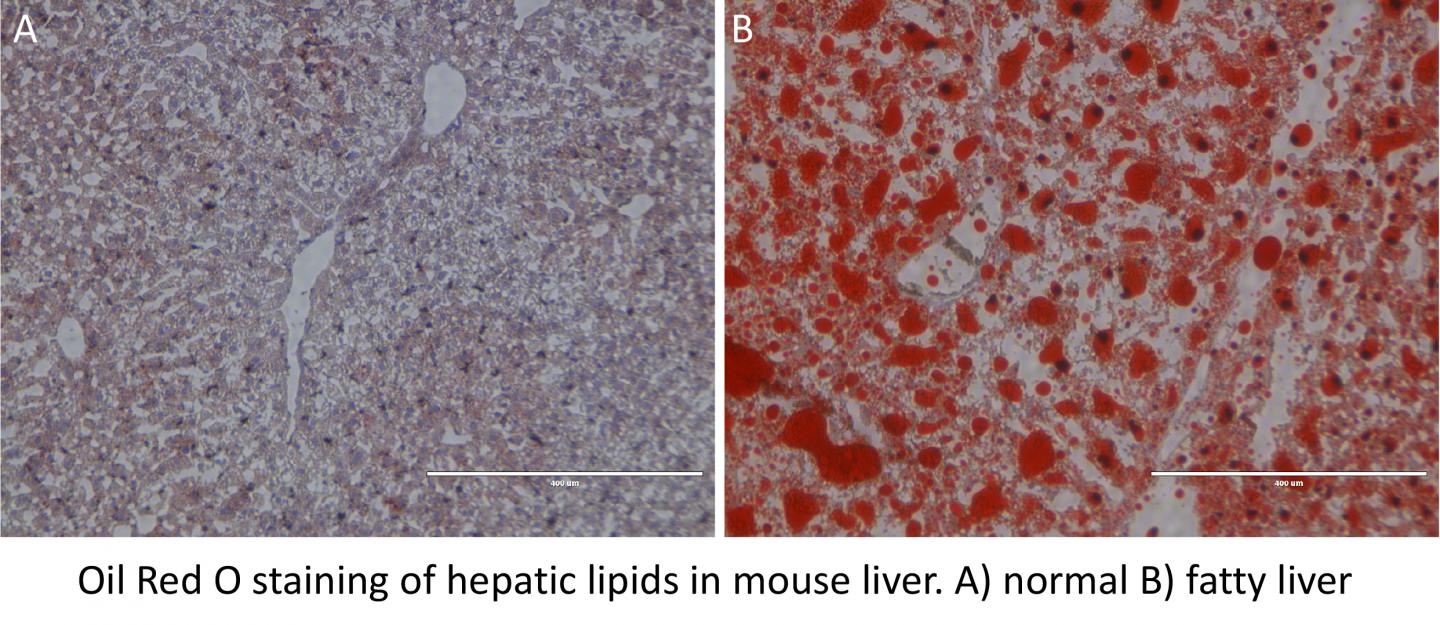
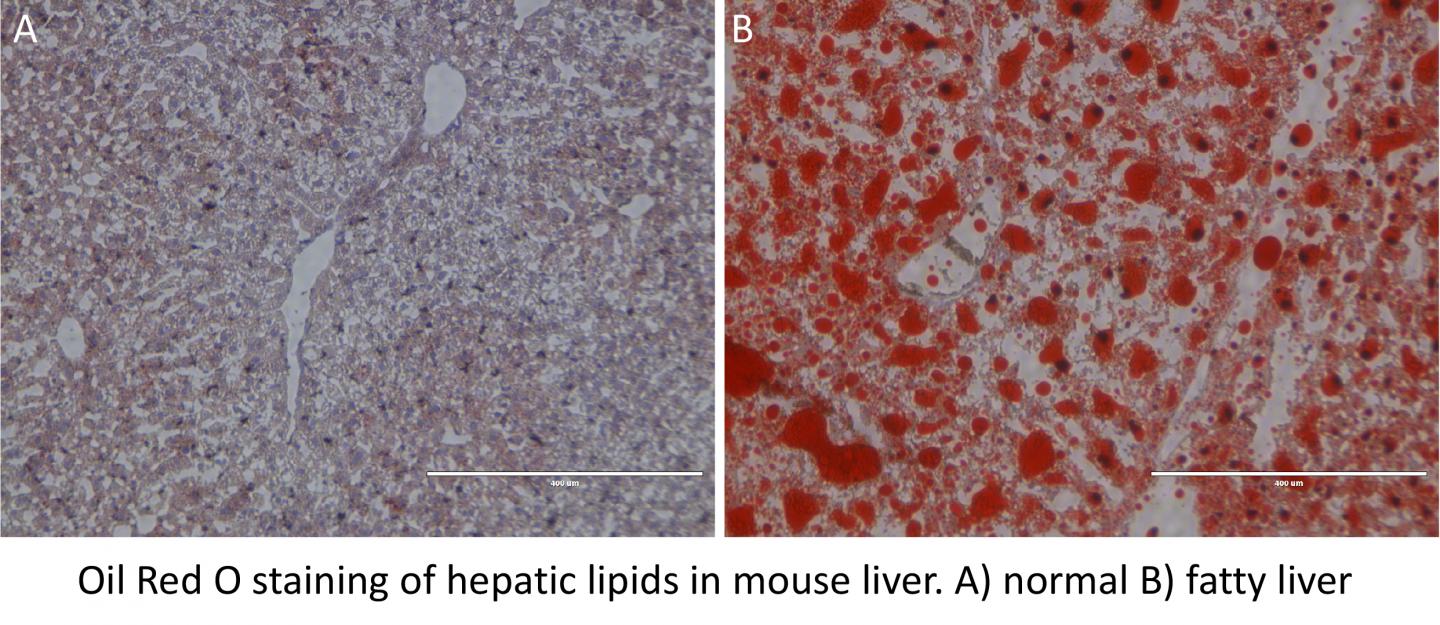
In mice, the absence of mTORC1 in liver cells caused a build-up of triglycerides in the liver, thereby reducing circulating triglycerides. On the other hand, activation of mTORC1 depleted liver triglycerides and increased blood triglycerides. Titchenell identified an important cellular process controlled by mTORC1 and demonstrated that mTORC1 controls the production of another class of molecules called phospholipids, which are essential for the triglyceride export from the liver. Phospholipids are necessary to form a barrier around triglyceride molecules allowing for their export and transport throughout the body.
"In insulin-resistant disorders such as diabetes and obesity, hyperactive mTORC1 in liver leads to excess fat production and export," Titchenell said. "mTORC1 is what we want to target pharmacologically to decrease the risk of cardiovascular disease that is associated with obesity and diabetes. If we could affect mTORC1 in a balanced way, then maybe could help prevent non-alcoholic fatty liver disease and heart disease."
In the future, the researchers aim to unravel the precise mechanisms that mediate mTORC1's control of phospholipid synthesis to uncover novel drug targets with the goal of reducing the excess lipid burden during metabolic disease.
###
This work was supported by the National Institutes of Health (R01 DK056886, K01 DK111715, T32 DK007314), the Samuel Chiaffa Memorial Fund, and the American Diabetes Association.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $6.7 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 20 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $392 million awarded in the 2016 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center — which are recognized as one of the nation's top "Honor Roll" hospitals by U.S. News & World Report — Chester County Hospital; Lancaster General Health; Penn Wissahickon Hospice; and Pennsylvania Hospital — the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2016, Penn Medicine provided $393 million to benefit our community.
Media Contact
Karen Kreeger
[email protected]
215-459-0544
@PennMedNews
http://www.uphs.upenn.edu/news/