Credit: N/A
In efforts to develop new treatments for brain cancer, scientists from Johns Hopkins Drug Discovery and the Kimmel Cancer Center's Bloomberg~Kimmel Institute for Cancer Immunotherapy report they have altered the structure of an experimental drug that seems to enhance its ability to slip through the mostly impermeable blood-brain barrier. Results of their proof-of-concept experiments in monkeys, published Aug. 25 in the Journal of Medicinal Chemistry, show a tenfold better delivery of the drug to the brain compared with the rest of animals' bodies.
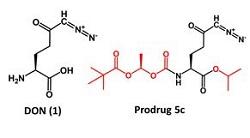
The scientists began with an experimental anti-cancer drug cultivated from bacteria found in Peruvian soil more than 70 years ago. Called 6 diazo-5-oxo L norleucine, or DON, the drug blocks the cellular use of the protein building block glutamine. On its own, DON has shrunk tumors in clinical trials of people with a variety of advanced cancers, but its damage to the gastrointestinal system, a glutton for glutamine, ultimately proved too toxic for humans, say the scientists.
"We wondered whether we could make a safer and more tolerable form of DON by enhancing its brain penetration and limiting its exposure to the rest of the body and, thus, toxicity," says Barbara Slusher, Ph.D., professor of neurology, medicine, psychiatry, neuroscience and oncology at the Johns Hopkins University School of Medicine and director of Johns Hopkins Drug Discovery.
Slusher teamed up with Johns Hopkins Kimmel Cancer Center immunologist Jonathan Powell, M.D., Ph.D., who has studied how cancer cells use different metabolic pathways to evade destruction by immune cells.
"A tumor uses aggressive metabolism to grow, sucking up all the surrounding nutrients, which leads to a very oxygen-poor, acidic environment that is not conducive to cancer-killing immune cells," says Powell, who is an associate director of the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
Powell suspects that using glutamine-blocking drugs to target tumor metabolism could make the environment around a tumor less harsh, slow down its growth and give the immune system a chance to attack the cancer cells. "The hope is to enhance certain immunotherapy drugs by adding such glutamine antagonists," says Powell.
To alter DON, Slusher and her drug discovery team designed and synthesized various derivatives, focused on making the drug more lipid soluble, or lipophillic, a trait known to aid passage through the blood-brain barrier. Once inside the brain, the new derivatives are designed to rapidly metabolize back to DON.
They gave DON and an altered derivative, dubbed 5c, intravenously to two monkeys and, 30 minutes later, measured the amount of the drugs in the monkeys' cerebrospinal fluid and circulating plasma, which is the liquid portion of blood that remains after blood cells, platelets and other cellular components are removed. The monkey that received DON had about seven times less concentration of the drug in its blood than the monkey that received 5c. In the monkey that received 5c, which converts to DON in the brain, the scientists found 10 times more DON in the cerebrospinal fluid than the monkey treated with unaltered DON.
"We showed that we can modify these drugs to have further specificity to target the brain and limit toxicity to the rest of the body," says Slusher. "This strategy can potentially be used to develop tailored drugs for different cancers."
###
This research was supported by a Technology Development Corporation (TEDCO) Maryland Innovation Initiative award and the Bloomberg~Kimmel Institute for Cancer Immunotherapy at Johns Hopkins and was performed in collaboration with the Institute of Organic Chemistry and Biochemistry of the Academy of Sciences of the Czech Republic.
Other scientists contributing to this research include Rana Rais, Michael Nedelcovych, Jesse Alt, Judson Englert, Camilo Rojas, Anne Le, Amira Elgogary, Jessica Tan, Kelly Pate and Robert Adams from Johns Hopkins; Dana Ferraris from McDaniel College; and Pavel Majer, Andrej Jancar?í?k, Lukas??Tenora and Lenka Monincova from the Czech Academy of Sciences.
Dracen Pharmaceuticals Inc. intends to license technology discussed in this publication from the Johns Hopkins University. Drs. Slusher, Powell and Rais are founders of and hold equity in Dracen Pharmaceuticals Inc. This arrangement has been reviewed and approved by the University in accordance with its conflict of interest policies.
Media Contact
Vanessa Wasta
[email protected]
410-614-2916
@HopkinsMedicine
http://www.hopkinsmedicine.org