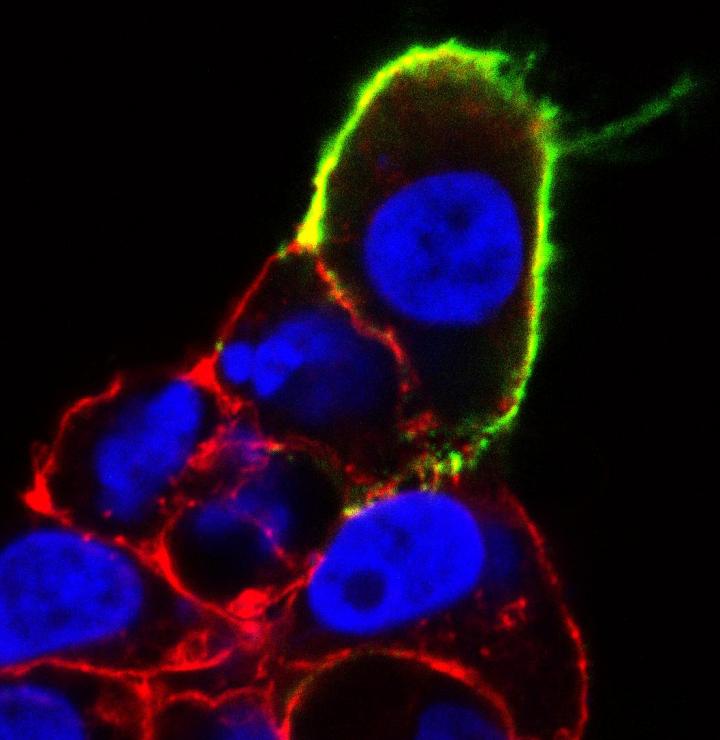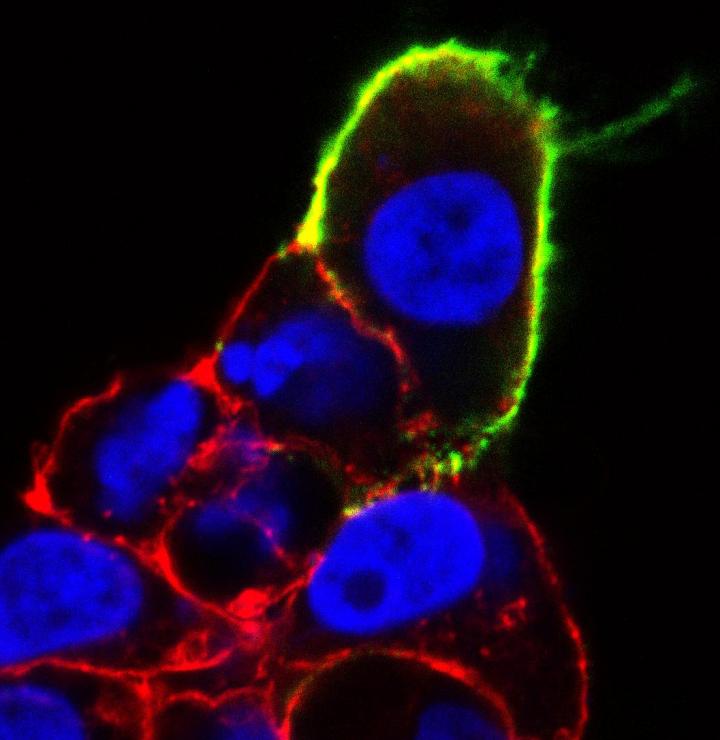
Credit: Kathleen Caron Lab, UNC
Like a bank robber on the lam, Gpr182 had assumed a variety of identities over several decades: G10D, HrhAMR, Gamrh, 7TMR, ADMR. Unable to put a finger on what exactly the gene does, scientists largely left it alone. The protein it codes for was designated an "orphan" receptor — a lock on the surface of cells without a known key.
In a study published today in the Journal of Clinical Investigation, it seems scientists have caught up with Gpr182 at last. Although the key that unlocks the Gpr182 receptor remains unknown, the study reveals a great deal about what's behind the door.
The findings suggest that if we can find a way to jimmy the lock, Gpr182 could prove a promising avenue for fighting cancers of the gastrointestinal tract.
"What makes this so exciting is that it's completely new," said Kathleen Caron, PhD, professor and chair of the department of cell biology and physiology in the UNC School of Medicine, who oversaw the research. "There was absolutely nothing known about this protein. I think these findings will be picked up on quickly, and I imagine it's going to fuel a lot of research on this receptor now."
The results are particularly tantalizing from a pharmaceutical perspective because they shed light on a new G-protein coupled receptor, a class of cell-membrane proteins well suited for drug development. About 40 percent of approved drugs target G-protein coupled receptors. The discovery of this new receptor could prove a promising lead for better understanding gastrointestinal biology and improving treatments for diseases such as colorectal cancer, the second leading cause of cancer-related deaths in the United States.
The study also shows that science is as much about asking questions as finding answers.
A fresh look at an old mystery
Caron's lab studies the cellular functions involved in cardiovascular health. What piqued her interest in Gpr182 was the common conception–a misconception, it turns out — that it is a receptor for the hormone adrenomedullin, which is thought to be instrumental in cardiovascular function. Scientists had put forth this notion after they conducted a few rat studies, but it had never been definitively confirmed.
"Of all the names it had over the years, the name that stuck was adrenomedullin receptor, or ADMR," said Caron, senior author of the paper and member of the UNC Lineberger Comprehensive Cancer Center. "It sort of hung that way in the databases for a while, even as science moved forward and scientists found another receptor that is considered to be the real adrenomedullin receptor. A few labs looked at this protein and sort of scratched their heads, because it wasn't really doing what an adrenomedullin receptor should be doing. And then everyone sort of dropped it for a good dozen years."
In the scientific literature, Gpr182 was a virtual nobody. Even now, a search of the PubMed database yields just two papers involving the gene. Given recent advances in scientific tools, Caron decided to attempt to finally pin down the fugitive gene.
Her team combined a commercially-available mouse model and a special "reporter" molecule to tag expression of Gpr182 in mice of different stages of development. The result was a precise map of where, and when, the Gpr182 receptor appears.
Tales from the (intestinal) crypt
The mapping experiment showed Gpr182 on cell surfaces in a handful of organs, including the kidney, lung and heart–but also, notably, in stem cells within the tube-like depressions that line the intestine, known as the intestinal crypt.
For a lab focused on the cardiovascular system, an intriguing lead in intestinal stem cells was somewhat off-target. But to Daniel Kechele, PhD, then a graduate student in Caron's lab, it looked like paydirt.
"In my undergraduate experience I had been in a gastrointestinal lab, and seeing that position within the intestinal crypt really sparked my interest," recalled Kechele, who is now a postdoctoral fellow at Cincinnati Children's Hospital. "My gastrointestinal background and the strong intestinal stem cell group at UNC made it possible to follow that lead and see where it would take us."
The stem cells of the intestinal crypt have been the focus of intense research because they represent an extreme version of the delicate balancing act between health and cancer. As food passes through the gastrointestinal tract, the cells lining the gut are constantly being sloughed off. To replenish them, the intestinal crypt stem cells must churn out, in humans, the equivalent of more than 100 square feet of cells to completely replace the gut lining about every seven days.
But this rapid proliferation is risky business. Too little, and a weak intestinal lining invites infection. Too much, and tumors form. Understanding the levers that intestinal stem cells use to regulate cell proliferation could shed light on cancer formation and lead to new treatments. Kechele wondered: Could Gpr182 be one of those levers?
Putting the brakes on proliferation
To find out, the team needed help. Fortunately, experts in stem cells, gastroenterology and cancer were right on UNC's campus — and eager to lend a hand. The researchers recruited an interdisciplinary team at UNC that included Scott Magness, PhD, Charles Perou, PhD, and Kay Lund, PhD, among others.
Particularly serendipitous was the fact that Scott Magness's lab had, in recent years, pioneered the development of an experimental tool the team would need to trace the gene's activity in intestinal stem cells. "This tool opened up a whole new world," Magness said. "All of a sudden we can use it to figure out how various genes of interest, like Gpr182, are expressed in both active and reserve stem cells, and how the gene might be functioning."
In their experiments with Magness's group, the researchers found that when Gpr182 was suppressed, cellular proliferation tended to increase, suggesting Gpr182 functions as a "brake" to keep proliferation in check. A mutation that suppresses Gpr182 could lead cells to proliferate a bit more freely, perhaps pointing to a link with cancer.
"We don't necessarily think this gene is itself a driver of cancer, but it's possible that mutations in the gene could play a role in the severity of the cancer," said Kechele.
On the flip side, suppressing Gpr182 could be beneficial in some situations. For example, when the researchers wiped out a mouse's active intestinal stem cell population with radiation (mimicking what happens during chemotherapy or radiation treatment), suppressing Gpr182 unleashed a marked increase in proliferation from the reserve stem cell population.
"That suggests this gene could be a target for therapy to speed up the regeneration of the gut lining after cancer treatment," said Magness. "By decreasing the expression of the Gpr182 protein, you might be able to induce the stem cells to respond more robustly in the regenerative phase, thus allowing doctors to use a higher or more effective therapeutic dosage without harming the normal functioning of the gut."
A promising drug target
To complement their studies in mice, the team also probed the links between Gpr182 and cancer in people. They found that expression of Gpr182 was significantly lower in the colons of patients with colorectal cancer compared with healthy colon tissue. Further analysis showed reduced Gpr182 expression in breast, lung and several other types of cancer, as well.
Together, the study findings suggest that manipulating Gpr182 expression or activation could offer a new avenue for cancer treatment, particularly for cancers or treatments that affect the gastrointestinal tract. One pharmaceutical company, Omeros, already purports to have developed a small molecule that interacts with Gpr182, a lead that could help speed drug development.
For Caron, the findings represent both an enticing new opportunity for biomedicine and a case study in the nature of science.
"I think it shows how passion and grit can really drive science in new and unexpected ways," said Caron. "It takes perseverance to keep asking questions and exploring things. If we had kept on assuming this was an adrenomedullin receptor, we would be missing the mark–and might have missed this exciting breakthrough."
###
Magness is an associate professor of medicine, cell biology and physiology, and biomedical engineering at the UNC School of Medicine. Perou is the May Goldman Shaw Distinguished Professor of Molecular Oncology and professor of genetics and pathology and laboratory medicine at the UNC School of Medicine. Lund is the Sarah Graham Kenan Distinguished Professor of Cell Biology and Physiology, with joint appointments in the departments of pediatrics and nutrition in the UNC School of Medicine. All are members of the UNC Lineberger Comprehensive Cancer Center.
The National Institutes of Health Funded this work.
Media Contact
Mark Derewicz
[email protected]
984-974-1915
@UNC_Health_Care