Biologists have discovered how an outer shield over T-type channels change the electrochemical signaling of heart and brain cells. Understanding how these shields work will help researchers eventually develop a new class of drugs for treating epilepsy, cardiovascular disease and cancer.
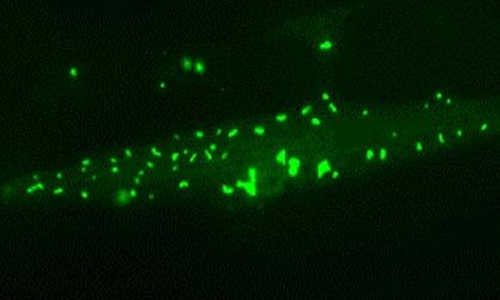
T-type channels in pond snails and other invertebrates are similar to those found in humans. Biologists have discovered how an outer shield over T-type channels change the electrochemical signaling of heart and brain cells. Photo Credit: University of Waterloo
The study from the University of Waterloo is published in the Journal of Biological Chemistry today and is featured as the “Paper of the Week” for its significance.
The researchers discovered T-type channels in the pond snail, Lymnaea stagnalis, can shift from using calcium ions to using sodium ions to generate the electrical signal because of an outer shield of amino acids called a turret situated above the channel’s entrance.
Low voltage T-type channels generate tiny pulses of current at regular intervals by selectively passing positively charged cations across the cell’s membrane through a gate-like channel. The channels are normally extremely selective, allowing just one sodium ion to pass for every 10,000 calcium ions.
The resulting rhythmic signals produced by this transfer of cations are what support the synchronous contraction of our heart muscles and neuronal firing in parts of the brain, like the thalamus, which helps regulate our sleep-wake cycle, or circadian rhythm.
In addition to their published findings, the researchers also found the shield-like turrets in pond snails restrict access of therapeutic drugs to the channel.
T-type channels in pond snails and other invertebrates are similar to those found in humans. Although pond snails reach only 7 cm in length, its simple neural network and physiology make it a popular model organism with neurobiologists.
Over-active T-type channels are linked to epilepsy, cardiac problems, neuropathic pain, as well as the spreading of several kinds of cancer. Drugs that could quench out-of-control T-type channel activity are unable to bind to the channels themselves.
“We wanted to understand the molecular structures of T-type channels,” said Spafford. “How they pass ionic currents to generate electrical activity, and to identify drug binding sites, and the drugs which may block these channels to treat neurological disease or heart complications.”
The group is currently investigating how dismantling this extracellular turret will improve drug access and binding in T-type channels.
Story Source:
The above story is based on materials provided by University of Waterloo.