Seven of 15 patients developed severe liver toxicity and died after taking a hepatitis B drug as part of a clinical trial in the early 1990s. Had a special variety of laboratory mouse been available then, that outcome could have been avoided, according to a study by researchers at the Stanford University School of Medicine.
Peltz’s Lab, Lab Members
A few years ago, Gary Peltz, MD, PhD, professor of anesthesia, in collaboration with researchers at the Central Institute for Experimental Animals in Kawasaki, Japan, developed a line of bioengineered mice whose livers were largely replaced with human liver cells that recapitulate the architecture and function of a human liver. Published experiments have shown that using these bioengineered mice enables researchers to detect drugs’ toxic metabolites and interactions with other drugs that do not occur in mouse livers. These would go unnoticed until human testing, and could produce severe adverse consequences in humans.
Now, Peltz and his fellow researchers have demonstrated that the drug administered in that tragic trial two decades ago — which an investigation conducted by the National Academy of Sciences determined had shown no signs of being dangerous during rigorous preclinical toxicology tests — causes severe liver toxicity when given to the bioengineered mice with humanized livers. This observation would have served as a bright red stop signal that would have prevented the drug from being administered to humans.
The researchers’ findings were published online April 15 in PLoS Medicine. Peltz is senior author of the paper. Postdoctoral scholar Dan Xu, PhD, is lead author.
Black-box warnings
Drug-induced liver injury is a major cause of liver-transplant demand in the United States and the leading cause of approved drugs’ being tagged with “black box” warnings on their labels or being pulled off the market entirely.
“The animals routinely used in preclinical tests for a drug’s toxicity have important differences from humans,” said Peltz, a former pharmaceutical executive who is intimately familiar with established preclinical testing procedures in the industry. “So when you take that drug into an early-stage clinical trial, you can be surprised.”
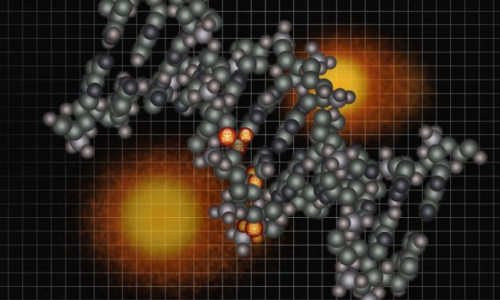
Probably the differences of greatest significance are in the liver. In addition to its numerous other job responsibilities, the liver is the primary organ for metabolizing drugs, chemically modifying them in various ways to make them easier for the body to get rid of. But some of those chemical products, or metabolites, can themselves be quite toxic if they reach high levels before they’ve been excreted. In fact, drug-induced liver damage is a major public-health problem, Peltz said.
For this reason, the Food and Drug Administration requires that prior to human testing, a drug’s toxological potential must be assessed in at least two mammalian species: one rodent and one nonrodent (such as a dog). But different animals given the same drug may process it quite differently. For example, human and mouse livers produce relatively different amounts of various metabolites from the same drug, so that a predominant metabolite in humans might be quite minor or totally absent in mice, and vice versa. A drug that in a human is converted at high rates to an extremely toxic metabolite may produce no such thing in another species’ livers, and slip through the cracks. While toxicity to humans is typically caught in early-stage safety tests, the numbers of participants can be too small and the durations too short for danger signs to begin flashing.
A drug’s promise
That’s what happened in 1993 when, after a short safety trial concluded without incident, the pharmaceutical giant Eli Lilly and Co. sponsored a phase-2 clinical trial of a drug for hepatitis B. The drug, called FIAU, was a member of a class of compounds called nucleoside analogs that partially mimic the chemical building blocks of genetic macromolecules such as DNA and RNA. Because this type of drug can interfere with viral replication, compounds such as FIAU were considered great candidates for ameliorating virally induced infections such as hepatitis B.
“FIAU was supposed to be a revolutionary drug,” Peltz said. “It looked very promising in preclinical tests. In phase 1, when the drug was administered to subjects for a short period of time, the human subjects seemed to do fairly well.” But the phase-2 trial was stopped after 13 weeks, when it became clear that FIAU was destroying patients’ livers. Before advancing to clinical trials, FIAU had been tested for as long as six months in mice, rats, dogs and monkeys without any trace of toxicity.
Some years ago, Peltz, working with scientists at the Central Institute for Experimental Animals under the direction of the late Tatsuji Nomura, MD, PhD, bioengineered mice by very selectively destroying most of their liver cells and repopulating the resulting cavity with human liver cells. The new cells took hold, multiplied and formed structures typical of the human organ. This was possible because these mice had deficient immune systems, so the human cells were not rejected. Studies have shown that these mice’s humanized livers express the same batteries of enzymes that human livers do and that they mimic the pattern of drug metabolism seen in human livers. Except for their impaired immune systems and altered livers, these mice are quite normal. That makes them ideal for liver-toxicity tests.
Turning back the clock
“When we first made these mice, my goal was to determine whether they could be a good model for predicting human toxicity,” Peltz said. Where better to demonstrate this than by turning back the clock to the preclinical toxicology studies that preceded the disastrous FIAU trial?
Peltz and his colleagues set out to determine how his bioengineered mice would fare in comparison with regular lab mice — the kind routinely used in clinical toxicology studies — when each type was given the drug. They administered four different doses of FIAU — which has never seen approval for any use since its failure in 1993 — once a day, orally (just as in the clinical trial), to a half-dozen or more mice of each type.
First they dosed the regular mice for four weeks, without eliciting symptoms of liver damage. “We could give them bucketsful of the drug, and there was no toxicity,” Peltz said. He and his team braced themselves for what they figured would be a long, drawn-out repetition with the bioengineered mice. “Within three days, the mice given the highest dose were mortally ill. They looked terrible, moved lethargically and ate poorly, just like people with liver trouble. By day four, we saw the same kinds of pathological lab results as had been seen in patients in that 1993 trial.” After two weeks, mice at lower doses showed the same clear signs of liver damage.
As a control, Peltz and his associates repeated their tests using a different drug called sofosbuvir, a member of the same drug class as FIAU that has, however, shown no evidence of liver toxicity in humans and was approved by the FDA in December 2013 for hepatitis C. Sure enough, the bioengineered mice given sofosbuvir did just fine, evincing no liver toxicity even at the highest administered dose.
“FIAU would never have been given to humans if it had first been tested on these mice,” Peltz said. “I really think they should be used before humans are exposed to new drugs.” The improved testing method has two advantages, he noted: First, as in the FIAU case, drugs that are selectively toxic in humans can be detected and a tragedy can be avoided. Second, we are less likely to lose a safe and effective drug that would be easily tolerated in a human liver due to “false-positive” signs of toxicity that can develop in nonhuman species.
Story Source:
The above story is based on materials provided by Stanford School of Medicine, BRUCE GOLDMAN.