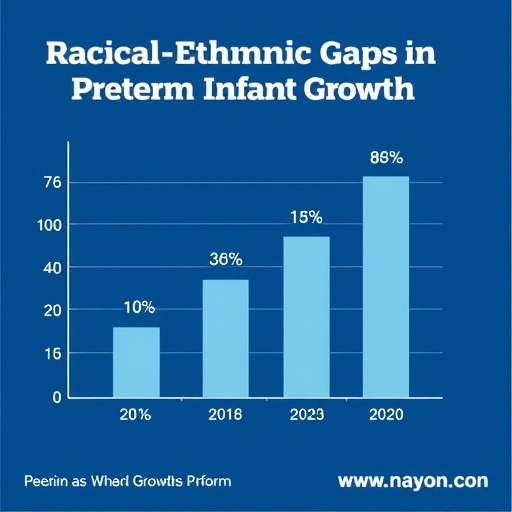
In the realm of neonatal care, understanding the intricacies of postnatal growth in preterm infants is paramount, especially when considering the nuanced impact of racial and ethnic disparities. A groundbreaking study recently published in the Journal of Perinatology spearheaded by researchers Chou, Yeh, and Hsueh et al. delves deeply into this issue, focusing on infants born before 30 weeks of gestation. The research aims to unravel disparities in birth weight (BW), the period it takes for infants to regain their birth weight, and the velocity of growth throughout the accelerated weight gain phase—a critical period for these vulnerable infants.
Preterm birth, especially before 30 weeks, poses significant challenges to infant survival and long-term development. The study reveals that racial and ethnic factors profoundly influence certain biometric parameters at birth and the subsequent growth trajectories in premature neonates. This comprehensive analysis utilized advanced statistical models and longitudinal cohort tracking to dissect differences between infants from diverse backgrounds, revealing patterns that raise essential clinical and social questions.
Birth weight, a fundamental metric for neonatal health assessment, emerged as a critical focal point in the study. The researchers identified marked variation in BW across racial and ethnic groups. These variations cannot be solely attributed to gestational age but also reflect complex interplays of genetic, environmental, and socioeconomic factors. The implications for neonatal intensive care units (NICUs) are profound, as birth weight consumption patterns influence immediate medical interventions and nutritional strategies.
Beyond the initial birth weight, the period required for infants to regain their BW stands as a vital indicator of early health stability and nutritional adequacy. The study meticulously documented that infants from certain racial and ethnic backgrounds experience a prolonged time to regain their birth weight. This delay may signify underlying disparities in postnatal care or differential vulnerability to complications such as feeding intolerance or infections. Understanding such differences is crucial for tailoring care protocols that address specific needs rather than adopting a one-size-fits-all approach.
Growth velocity during the accelerated weight gain phase represents a pivotal developmental milestone for preterm infants, who are often at risk for growth faltering. The study’s longitudinal approach allowed for a detailed assessment of mean growth velocity and its disparities across racial and ethnic groups. The findings suggest that infants’ capacity to achieve adequate growth velocity—and by extension, developmental potential—is intimately linked to their racial and ethnic background. This introduces questions about the interplay between genetic predispositions, nutritional access, and postnatal care environments.
Tracking the biological determinants of these disparities, the authors hypothesize a multifactorial etiology involving both innate and extrinsic factors. Genetic predispositions may influence metabolic efficiency and nutrient utilization, affecting growth rates postnatally. Simultaneously, social determinants such as healthcare access, maternal health status, and quality of neonatal nutrition are posited as significant contributors to the observed disparities.
This research also challenges existing neonatal growth standards, which predominantly derive from data collected on homogeneous populations. The implication is clear: standardized growth charts may inadequately represent diverse neonatal populations, potentially leading to misinterpretation of growth adequacy in minority infants. Developing customized growth norms that reflect racial and ethnic diversity could revolutionize neonatal care by enhancing diagnostic precision and therapeutic targeting.
Furthermore, the study underscores the urgent need to integrate racial and ethnic considerations into neonatal clinical trials and nutritional intervention programs. Tailored strategies may include individualized feeding protocols, culturally sensitive health education for caregivers, and enhanced surveillance for growth deviations in high-risk groups. Such steps are vital to mitigate disparities and promote equitable health outcomes from the outset of life.
Clinically, these findings serve as a catalyst for revisiting current NICU practices. Healthcare providers must heighten vigilance regarding growth trends in preterm infants, with an awareness of the potential for racial and ethnic biases in growth expectations. Interdisciplinary collaboration among neonatologists, dietitians, social workers, and epidemiologists will be necessary to develop and implement evidence-based, equity-focused care models.
Policy implications of this research are equally profound. Bridging gaps in postnatal growth within racially and ethnically diverse populations requires systemic shifts in healthcare accessibility, insurance coverage, and community support programs. Enhancing maternal and infant health equity could involve targeted funding for perinatal nutrition, improved prenatal care in minority communities, and comprehensive education campaigns addressing the specific needs of these populations.
From a research standpoint, the study by Chou and colleagues opens avenues for further exploration into biological mechanisms underlying growth disparities. Future investigations might explore epigenetic modifications, nutrient metabolism pathways, and the role of the microbiome in influencing neonatal growth patterns. Such multidisciplinary research efforts will deepen understanding and yield novel interventions.
The intersection of genetics, environment, and social determinants in shaping postnatal growth trajectories presents a complex challenge but also an opportunity for innovation in neonatal medicine. By embracing this complexity, healthcare systems can move beyond generalized care paradigms and aim for precision medicine approaches that recognize the uniqueness of each infant’s background and needs.
In conjunction with advancements in neonatal nutrition and respiratory care, addressing racial and ethnic disparities is critical for improving survival and long-term developmental outcomes in preterm infants. The study illustrates that growth velocity and birth weight regain are not merely clinical parameters but markers of broader systemic health equity issues that must be confronted.
This paradigm shift aligns with broader public health goals aimed at reducing infant mortality and morbidity disparities. Mechanisms to implement findings into practice include enhanced data collection on race and ethnicity in neonatal records, formation of equity-centered care guidelines, and fostering community engagement to support vulnerable populations.
In summary, the work by Chou, Yeh, Hsueh, and their team provides crucial insights into the racial and ethnic disparities that shape postnatal growth in infants born before 30 weeks of gestation. Their rigorous methodology and comprehensive analysis lay the groundwork for transforming neonatal care and highlight the necessity of integrating equity into every aspect of health delivery.
As neonatal medicine evolves, incorporating the social and biological dimensions of health will be indispensable for achieving better outcomes. This pioneering research is an essential step on that road, urging clinicians, researchers, and policymakers alike to address disparities proactively and innovatively.
The journey toward equitable neonatal outcomes demands the collaboration of diverse stakeholders, unified by the goal of ensuring every infant, irrespective of racial or ethnic background, has the opportunity for optimal growth and development. The study’s findings will undoubtedly resonate across disciplines, spurring dialogue and action for a more just health future.
Subject of Research: Racial and ethnic disparities in postnatal growth of infants born before 30 weeks of gestation.
Article Title: Racial and ethnic disparities in postnatal growth of infants born before 30 weeks of gestation.
Article References:
Chou, FS., Yeh, HW., Hsueh, C. et al. Racial and ethnic disparities in postnatal growth of infants born before 30 weeks of gestation. J Perinatol (2026). https://doi.org/10.1038/s41372-026-02570-8
Image Credits: AI Generated
DOI: 04 February 2026
Tags: advanced statistical models in neonatal researchbirth weight variations in preterm infantschallenges of preterm birth before 30 weekscritical weight gain phases in preterm infantsethnic influences on infant developmentimpact of ethnicity on preterm infant outcomesimplications for neonatal care policieslongitudinal studies on infant growthneonatal health disparitiespreterm infant growth trajectoriesracial disparities in neonatal careracial-ethnic disparities in healthcare