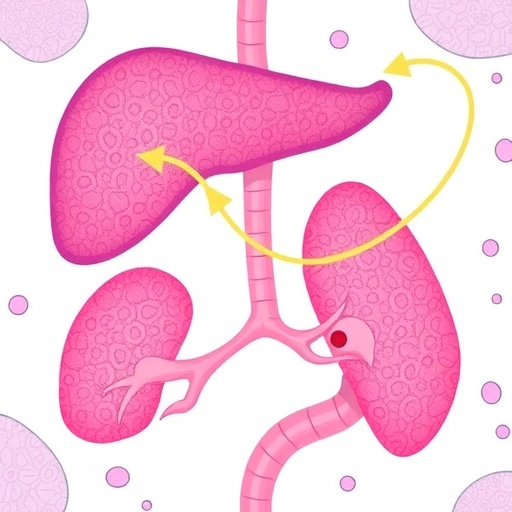
A groundbreaking study published in the Journal of Translational Medicine reveals a compelling new axis in the realm of hepatocellular carcinoma (HCC) metabolism, namely the HKDC1-ASS1-ACSBG2 pathway. Hepatocellular carcinoma is notoriously challenging to treat due to its resistance to conventional therapies, and this research sheds light on the underlying mechanisms that fuel such resistance. Understanding the metabolic pathways in cancer cells is essential, as these pathways often aid in tumor progression and therapy evasion. The study delineates how the interactions among these three proteins play a pivotal role in promoting lipid metabolism that ultimately contributes to therapeutic failure in HCC.
Early investigations into the HKDC1-ASS1-ACSBG2 axis highlighted the role of HKDC1 (hexokinase domain-containing protein 1) in facilitating glucose metabolism. This protein is known for its capacity to support energy production in cancer cells, which typically rely on glycolysis, a process that allows them to thrive even in low-oxygen environments. The upregulation of HKDC1 has been associated with aggressive tumor phenotypes, further elucidating its role in the metabolic reprogramming of HCC. Investigators have postulated that targeting this protein could enhance the effectiveness of standard therapies by cutting off an essential energy supply to the tumor.
The second player in this triad is ASS1 (argininosuccinate synthase 1), a critical enzyme involved in the urea cycle. In many cancers, including hepatocellular carcinoma, ASS1 expression is frequently reduced, leading to an accumulation of nitrogenous waste. This deficiency modifies metabolic pathways, causing a shift that can support rapid tumor growth. As ASS1 levels drop, alternative metabolic pathways are initiated, allowing cancer cells to adapt and survive even under therapeutic stress. The insights into ASS1’s involvement in HCC metabolism are revolutionary, suggesting that restoring its function could diminish cancer cell resilience.
ACSBG2 (acyl-CoA synthetase bubblegum family member 2) further complicates the metabolic interplay within HCC. As an important regulator of fatty acid metabolism, ACSBG2 facilitates the conversion of acyl-CoAs and supports lipid biosynthesis, both of which are crucial for membrane synthesis in rapidly dividing cancer cells. Elevated fatty acid levels can promote cell proliferation and contribute to the tumor microenvironment’s metabolic heterogeneity. The paper discusses ACSBG2’s role in enhancing lipid metabolic pathways, which, when activated in conjunction with HKDC1 and ASS1 downregulation, creates an advantageous scenario for HCC progression and therapeutic resistance.
Through a series of well-designed experiments, the researchers demonstrated that inhibiting any one of the components in the HKDC1-ASS1-ACSBG2 axis led to significant changes in the metabolic profile of HCC cells. When HKDC1 was silenced, a decrease in cell proliferation was observed, accompanied by a shift in key metabolic pathways. Similarly, inhibiting ASS1 affected the metabolic flexibility of the cells, forcing them to rely more heavily on glycolysis and lipid metabolism. This mutual dependence among the three proteins underscores a complex but important dynamic in how HCC cells may outsmart treatment regimens.
As the study progresses, the authors also examined potent inhibitors that target these metabolic pathways to assess their efficacy as adjunct therapies in HCC management. The combination of metabolic inhibitors with traditional therapies holds promise, suggesting a simultaneous strategy to tackle therapeutic resistance. This combined approach may potentially reverse the adaptive changes in metabolism that cancer cells exploit, laying the groundwork for more effective treatment strategies in the management of hepatocellular carcinoma.
Future research directions are outlined, which include identification and testing of specific inhibitors that can dismantle the HKDC1-ASS1-ACSBG2 axis. Moreover, there is a push for further exploration into the implications of metabolic reprogramming in other types of cancers. The metabolic symbiosis exhibited by cancer cells highlights a critical avenue for intervention that could change the trajectory of cancer treatment overall. This study serves as a beacon for oncologists and scientists alike, potentially leading to therapeutic breakthroughs that enhance patient outcomes.
Collectively, these findings establish a robust connection between lipid metabolism and therapeutic resistance in hepatocellular carcinoma. The nuanced interactions between HKDC1, ASS1, and ACSBG2 provide not only a solid scientific basis for future investigations but also a narrative that emphasizes the importance of understanding cancer metabolism in the fight against resistant tumors. By unveiling this metabolic nexus, the authors have potentially opened new doors for innovative cancer therapies that specifically target metabolic vulnerabilities, offering hope for HCC patients facing dire prognoses.
In summary, the HKDC1-ASS1-ACSBG2 axis signifies a novel convergence of metabolic processes in HCC that extend beyond traditional therapeutic paradigms. The interplay of these molecules illustrates a vital aspect of cancer biology that needs to be understood more thoroughly to develop precise interventions. This study adds a significant layer to our comprehension of tumor metabolism, steering a new research horizon while forecasting an innovative approach to tackle the menacing challenge of therapeutic resistance in cancer treatment.
Subject of Research: Metabolic pathways in hepatocellular carcinoma and their role in therapeutic resistance.
Article Title: The HKDC1-ASS1-ACSBG2 axis reprograms lipid metabolism to drive therapeutic resistance in hepatocellular carcinoma.
Article References:
Ling, X., Zhao, W., Li, K. et al. The HKDC1-ASS1-ACSBG2 axis reprograms lipid metabolism to drive therapeutic resistance in hepatocellular carcinoma. J Transl Med (2026). https://doi.org/10.1186/s12967-026-07779-x
Image Credits: AI Generated
DOI: 10.1186/s12967-026-07779-x
Keywords: Hepatocellular carcinoma, lipid metabolism, therapeutic resistance, metabolic pathways, HKDC1, ASS1, ACSBG2.
Tags: aggressive tumor phenotypescancer metabolism pathwaysenhancing cancer therapy effectivenessglucose metabolism in cancer cellsHepatocellular carcinoma resistancehexokinase domain-containing protein 1HKDC1-ASS1-ACSBG2 pathwayJournal of Translational Medicine studylipid metabolism in tumorsmetabolic reprogramming in cancertargeting cancer energy supplytherapeutic failure in HCC