In recent years, the opioid crisis has surged into one of the most devastating public health emergencies worldwide, profoundly impacting millions of lives. A new population-based study, recently published in the International Journal of Mental Health and Addiction, sheds critical light on the survival odds of those hospitalized due to opioid-related incidents and reveals a nuanced understanding of how socioeconomic status (SES) influences these outcomes. This research not only quantifies survival probabilities but also uncovers the socioeconomic disparities that compound the crisis, opening a pivotal dialogue about targeted interventions.
Hospitalizations following opioid overdose incidents serve as an urgent marker, signaling the severe health consequences faced by affected individuals. The survival rates post-hospitalization are crucial metrics, informing clinicians and policy-makers alike about the effectiveness of current medical and social interventions. This study meticulously analyzed a comprehensive dataset encompassing a diverse population, providing an unprecedented scale of epidemiological insight. By focusing specifically on how SES factors modulate survival chances, the researchers have pinpointed vulnerabilities that often remain obscured in broader statistical analyses.
The investigation spans an extensive cohort, integrating data from healthcare facilities, socioeconomic demographic databases, and mortality records. This multidisciplinary approach enabled the authors to categorize patients not only by their clinical presentations and treatment pathways but also by income brackets, education levels, employment status, and community deprivation indices. Such granular stratification allowed the identification of survival disparities tied to socioeconomic stratification, emphasizing that the opioid epidemic is as much a social issue as it is a medical one.
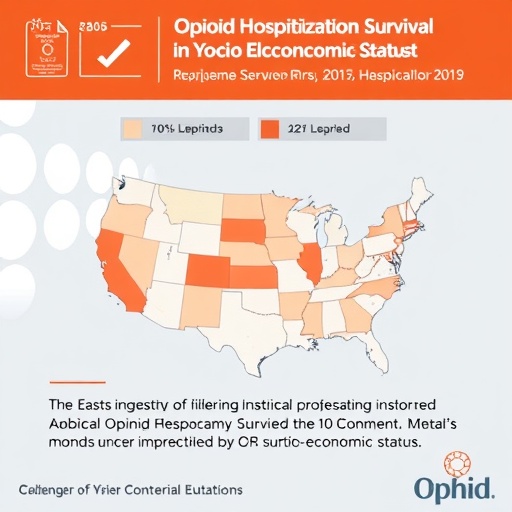
One of the hallmark findings of this research is the stark contrast in survival probabilities between lower and higher SES groups. Patients from economically disadvantaged backgrounds exhibited significantly lower rates of survival after opioid-related hospitalization, a disparity that persisted even after adjusting for factors such as age, gender, and comorbidities. This revelation suggests that beyond the immediate medical emergency, the broader social determinants of health significantly influence recovery trajectories and long-term outcomes.
These results align with prior epidemiological evidence suggesting that socioeconomic disadvantage is associated with reduced access to healthcare resources, suboptimal engagement with follow-up care, and increased exposure to stressors that may exacerbate substance use disorders. Notably, the study highlights that individuals in lower SES brackets may face barriers such as unstable housing, diminished social support, and limited access to addiction treatment programs, all of which can culminate in poorer survival and higher risk of relapse or subsequent overdose.
Technically, the researchers employed survival analysis techniques, including Kaplan-Meier curves and Cox proportional hazards models, to robustly characterize and compare survival across socioeconomic strata. This rigorous statistical framework ensures that conclusions about SES impacts are not confounded by other clinical variables, providing a clear demonstration of how social conditions alone modulate survival probabilities. The study’s methodology reflects an advanced integration of biostatistical modeling with social epidemiology, setting a benchmark for future research.
Furthermore, the study explores temporal trends in survival, revealing that improvements in hospital care and overdose interventions have modestly increased survival rates overall. However, these improvements have not been equitably distributed. High SES groups have benefited disproportionately, emphasizing the urgent need to tailor public health initiatives towards the most vulnerable and marginalized populations, whose outcomes remain dismal despite medical advances.
Implications of these findings are profound. They advocate for multi-level interventions that extend beyond immediate hospital care. Strategies that target underlying socioeconomic barriers—such as expanding access to stable housing, enhancing community-based support systems, and ensuring comprehensive addiction treatment regardless of insurance status—are essential to genuinely leveling the survival field. In this light, public health policies should pivot toward inclusivity and equity, recognizing the multifaceted nature of the opioid epidemic.
Moreover, the study underscores the essential importance of integrating social determinants frameworks into clinical practice. Physicians and healthcare providers need to assess not only the clinical severity of an opioid overdose but also the socioeconomic contexts to which patients will return upon discharge. Tailored discharge planning, incorporating social work and case management, could improve adherence to follow-up treatment protocols and reduce fatal outcomes. This holistic approach promises to bridge the gap between acute care and long-term recovery.
Scholars and policymakers scrutinizing this study will find a robust call to action in its conclusions. Addressing opioid-related mortality requires coordinated efforts at community, institutional, and governmental levels. This includes funding for harm reduction programs, advancement of equitable healthcare policies, and investments in public education to dismantle stigma surrounding substance use disorders, which often disproportionately affects marginalized socioeconomic groups.
The interplay of SES with opioid survival also invites further scientific inquiry. Future research may delve into biological and psychological mediators that link socioeconomic disadvantage to worse outcomes, including the roles of chronic stress, mental health comorbidities, and genetic predispositions. Advanced data science tools such as machine learning could be employed to identify at-risk individuals preemptively, enabling proactive intervention.
This study marks a significant step forward in understanding how the opioid crisis is intertwined with social inequities. It challenges simplistic narratives that frame addiction solely as a consequence of individual behavior by providing compelling empirical evidence of systemic disparities. By shifting the discourse towards social determinants, the research offers hope for more effective, just, and sustainable solutions that can save lives across all strata of society.
In conclusion, the comprehensive analysis presented provides an indispensable resource for those grappling with the opioid epidemic’s complexity. As hospitalizations for opioid-related issues continue to climb globally, insights into survival dynamics and the impactful role of socioeconomic status are critical. The findings beckon a recalibration of public health priorities, with an urgent emphasis on social equity to turn the tide on opioid-related mortality.
The study, authored by Alsabbagh, Shah, Beazely, and colleagues, is poised to influence both clinical practice and health policy profoundly. Its meticulous approach and compelling conclusions represent a watershed moment in the literature, illuminating pathways to save lives and reduce disparities in a crisis that touches every community in some capacity. As efforts intensify to combat opioid mortality, integrating socioeconomic considerations as demonstrated here will be indispensable for meaningful progress.
Subject of Research: Survival outcomes following opioid-related hospitalizations and the impact of socioeconomic status on survival rates.
Article Title: Survival After Opioid-Related Hospitalization and the Impact of Socioeconomic Status (SES) on Survival: A Population-Based Study.
Article References:
Alsabbagh, M., Shah, NUH., Beazely, M.A. et al. Survival After Opioid-Related Hospitalization and the Impact of Socioeconomic Status (SES) on Survival: A Population-Based Study. Int J Ment Health Addiction (2026). https://doi.org/10.1007/s11469-025-01619-7
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11469-025-01619-7
Tags: comprehensive dataset analysis in public healthdisparities in opioid-related health outcomesepidemiological insights into opioid addictionhealthcare disparities and addiction treatmenthospitalizations due to opioid overdosemultifactorial approach to opioid crisis solutionsopioid crisis impact on healthpopulation-based study on opioid hospitalizationsocioeconomic factors in health crisessocioeconomic status and survival ratessurvival probabilities after opioid incidentstargeted interventions for opioid addiction