In recent years, the integration of 3D printing technology in the medical field has emerged as a revolutionary force, providing unprecedented opportunities for improving surgical training and patient outcomes. A notable area of research within this domain is the evaluation of simulators used for emergency procedures, as exemplified by a recent study conducted by Wegner et al., which compares conventional training simulators to their 3D printed counterparts for emergency percutaneous cricothyrotomy. This procedure, which often serves as a life-saving intervention in cases of airway obstruction, underscores the importance of effective training methods for healthcare professionals.
The randomized controlled trial conducted by Wegner and collaborators provides critical insights into the efficacy of different training simulators. Traditional simulators have long been utilized in medical training, relying on standard materials and construction methods. However, with the advent of 3D printing technology, it is now possible to create highly customizable simulators that can replicate the nuances of human anatomy with remarkable accuracy. This study aims to elucidate whether these advanced simulators can significantly enhance the learning and performance of medical trainees as compared to conventional methods.
The methodology employed in this trial is noteworthy for its rigor and comprehensive approach. Participants were randomly assigned to receive training on either the conventional simulator or the 3D printed version, both equipped with two distinct training kits. This design not only allows for a direct comparison of the simulators themselves but also provides variability in the training experience, reflecting the complexities that can be encountered in real-world scenarios. By utilizing a randomized controlled trial design, the authors can draw stronger conclusions about the efficacy of each training method with reduced bias.
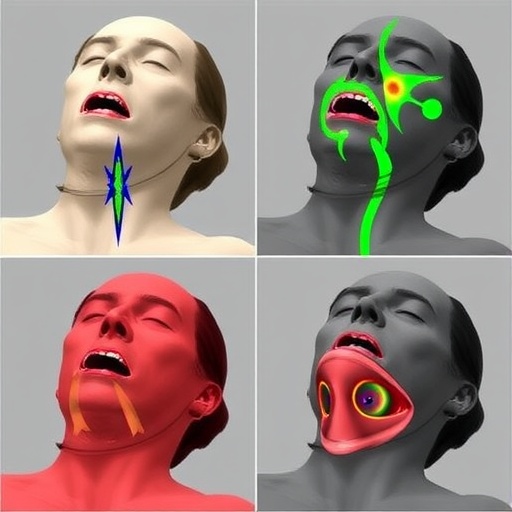
One of the intriguing aspects of this study lies in the technical specifications of the 3D printed simulator. Utilizing advanced additive manufacturing techniques, the researchers created a model that closely mimics the anatomical structures that a trainee would encounter during a cricothyrotomy. This includes not only the surface contours of the neck but also the internal structures, which are critical for successfully performing the incision. Such attention to detail ensures that the simulator serves as a true representation of the human anatomy, fostering a more effective learning environment.
In addition to the anatomical accuracy, the tactile feedback provided by the 3D printed simulator is another focal point of the study. Trainees often highlight the importance of feeling the resistance and texture of the tissues during training, as this sensory experience can greatly influence their readiness for real-life situations. By offering a more lifelike simulation, the 3D printed model potentially alters not only the learning curve but also the confidence levels of the trainees when faced with actual clinical emergencies.
The outcomes of the study were measured through a series of assessments, which included both performance evaluations and subjective feedback from the participants. These metrics are invaluable, as they not only quantify the technical skills acquired but also gauge the overall experience of the trainees with the simulators. Such feedback is crucial for further refining both the educational approach and the design of the training tools themselves. A better understanding of user experience can guide future research in simulator development and ultimately lead to improved training modalities.
Preliminary results indicate a marked improvement in performance among those who trained with the 3D printed simulator. Participants reported that they felt more prepared and capable in executing the emergency cricothyrotomy procedure, a finding that carries significant implications for emergency medicine training programs. If these results can be substantiated in larger cohorts and diverse training environments, the move towards integrating 3D technology in medical training could become not just a trend, but a standard practice.
Moreover, the cost-effectiveness of producing 3D printed simulators cannot be overlooked. While initial investments in 3D printing technology may pose challenges, the ability to rapidly produce customized training models can be a game-changer for institutions facing budget constraints. Rather than relying on expensive and often inflexible traditional simulators, medical education programs can leverage 3D printing to create a wide range of training tools tailored to their specific needs.
As medical education continues to evolve, the importance of adopting innovative teaching methods cannot be understated. The study by Wegner et al. emphasizes a shift in how training for high-stakes procedures is approached, advocating for the incorporation of cutting-edge technology in educational curricula. This research not only highlights the potential of 3D printed simulators but also serves as a catalyst for further exploration and development in the field of medical training.
In conclusion, the findings from this randomized controlled trial offer compelling evidence for the advantages of 3D printed simulators in emergency medicine training. As the medical community grapples with the need for effective and efficient training solutions, studies such as these provide a roadmap for future innovations. The integration of technology into medical education is poised to redefine training methodologies, resulting in better-prepared practitioners and ultimately better patient care.
As the demand for advanced medical training tools continues to rise, it will be essential for researchers, educators, and healthcare leaders to collaborate on developing and implementing strategies that harness the full potential of 3D printing technology. The journey towards enhancing medical education is not merely an academic endeavor; it represents a commitment to improving healthcare delivery and outcomes in an increasingly complex world.
Ultimately, as we reflect on the findings of Wegner et al., it becomes clear that the future of medical training lies in our ability to embrace innovation and adapt to the evolving landscape of healthcare education. By continuing to explore the capabilities of technologies such as 3D printing, we can pave the way for a new era of training that prioritizes both accuracy and practicality, ensuring that healthcare professionals are equipped with the skills necessary to navigate the challenges of their critical roles.
Subject of Research: Comparison of conventional versus 3D printed simulators for emergency percutaneous cricothyrotomy training.
Article Title: Comparing conventional versus 3D printed simulators for simulation training of emergency percutaneous cricothyrotomy with two different kits: a randomized controlled trial.
Article References:
Wegner, M., Dusse, F., Beeser, F. et al. Comparing conventional versus 3D printed simulators for simulation training of emergency percutaneous cricothyrotomy with two different kits: a randomized controlled trial.
3D Print Med (2026). https://doi.org/10.1186/s41205-026-00315-z
Image Credits: AI Generated
DOI: 10.1186/s41205-026-00315-z
Keywords: 3D printing, simulator, emergency medicine, medical training, cricothyrotomy.
Tags: 3D printing in medical trainingairway obstruction emergency procedurescomparing training simulators for healthcarecustomization in medical simulatorsefficacy of 3D printed medical simulatorsemergency cricothyrotomy simulationenhancing learning in medical traineesevaluation of cricothyrotomy training methodsimproving surgical training outcomesinnovative training technologies in healthcarerandomized controlled trial in medical educationtraditional vs advanced surgical training methods