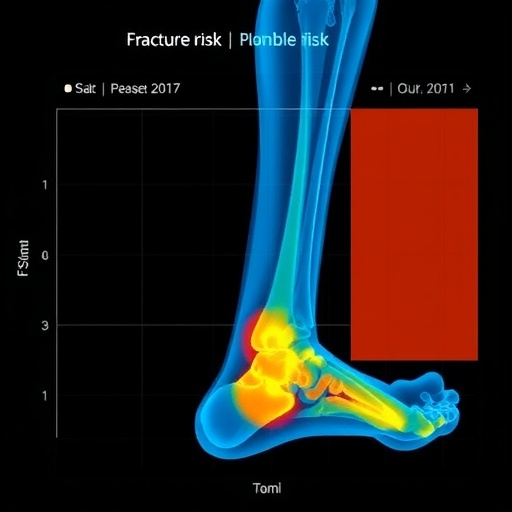
A groundbreaking study published in the journal Archives of Osteoporosis has introduced an innovative approach named FREMML, aimed at revolutionizing how healthcare providers identify individuals at imminent risk of fractures. This new decision-support system leverages advanced machine learning techniques, integrating multiple sources of patient data to forecast fracture risk with unprecedented accuracy. As populations age and the prevalence of osteoporosis rises, the demand for effective and proactive health interventions is more pressing than ever. The research conducted by Rietz, Brønd, Möller, et al., signifies a pivotal step in fracture risk management and may save countless lives.
The primary focus of FREMML is to utilize a comprehensive database that encompasses a wide array of clinical indicators, lifestyle factors, and demographic data. Traditional fracture risk assessments often rely on subjective interpretations of data or singular metrics such as bone mineral density, which can overlook critical factors influencing a patient’s overall risk. By employing machine learning algorithms, FREMML identifies patterns and correlations across diverse datasets, ensuring a more holistic understanding of each patient’s situation.
Central to the effectiveness of FREMML is its ability to process vast amounts of information far more rapidly and accurately than human practitioners could manage. Utilizing a blend of historical patient outcomes, genetic predispositions, and environmental influences, the algorithm can generate a risk profile for individual patients quickly. This rapid assessment allows for timely interventions that can significantly mitigate the potential for fractures, which can lead to serious complications, including disability and even mortality in older adults.
The development and deployment of FREMML are underscored by the urgent need for healthcare systems worldwide to transition to more data-driven models. The old paradigms of one-size-fits-all assessment tools have proven inadequate when addressing the unique complexities of fracture risk. FREMML not only enhances the precision of risk assessments but also empowers clinicians with actionable insights, equipping them to devise personalized prevention strategies tailored to individual patient profiles.
One of the most notable aspects of FREMML is its user-friendly interface. This design consideration ensures that healthcare providers, regardless of their technical expertise, can easily navigate the system to obtain crucial insights into fracture risks. With intuitive visualizations and recommendations, clinicians can make informed decisions that align with the latest clinical guidelines, further bridging the gap between technology and healthcare practice.
Moreover, FREMML addresses a critical issue in healthcare: the management of resource allocation. By identifying high-risk individuals accurately, healthcare systems can focus their efforts on preventive measures for those who need it most. This targeted approach not only enhances patient outcomes but also optimizes the utilization of medical resources, thereby reducing costs associated with managing fractures after they occur.
As the study highlights, the successful implementation of FREMML depends on collaboration between data scientists, healthcare providers, and policymakers. Creating a seamless integration of this technology within existing healthcare infrastructures requires a concerted effort from all stakeholders. The promise of improved patient outcomes creates a compelling case for this collaborative approach, with potential benefits extending into broader public health domains.
Importantly, the potential for FREMML to adapt and evolve is immense. Future iterations of the system could incorporate ongoing advancements in genomics and personalized medicine, ensuring that the technology remains at the forefront of fracture risk assessment. This adaptability aligns with trends in healthcare highlighting the significance of tailored treatment plans, shifting the focus from reactive to proactive health management.
In an era marked by technological innovation, it is crucial that the medical community embraces tools like FREMML. The intersection of artificial intelligence and medicine presents endless possibilities, and FREMML exemplifies how these advancements can lead to better health outcomes. As more researchers and institutions explore similar paradigms, the collective knowledge gained could foster an environment where personalized medicine thrives, ultimately benefiting a greater number of patients.
The implications of FREMML are not confined solely to fracture risk assessment. The fundamentally new approach it proposes could reshape how we think about chronic disease management as a whole. By establishing robust methodologies for risk prediction across various medical domains, FREMML sets a precedent that other areas of healthcare can learn from, potentially leading to improvements in treatment efficiency and patient care.
In conclusion, FREMML represents more than just an advanced tool for fracture risk assessment; it embodies a shift towards a more integrated and data-driven philosophy in medicine. As further research unfolds and the technology matures, its potential to influence strategies for injury prevention, especially among vulnerable populations, is both promising and revolutionary. The future of fracture risk management looks bright, thanks to the initiative led by Rietz and colleagues.
Achieving widespread adoption of FREMML will necessitate continuous evaluation and refinement. Future studies will undoubtedly play a vital role in assessing the efficacy of the model in real-world settings and its adaptability to diverse healthcare environments. With its promising inception, FREMML holds the possibility of becoming a gold standard in identifying and mitigating fracture risk, significantly impacting how healthcare professionals approach osteoporosis management.
As we move forward, maintaining an informed dialogue among healthcare practitioners, patients, and researchers will be essential in harnessing the full potential of FREMML and similar innovations. This collaborative effort will not only optimize the model itself but also enhance our understanding of fracture risks associated with aging and osteoporotic conditions. Ultimately, it is the collective aim of the medical community to create a healthier, more resilient population capable of living longer, fracture-free lives.
Subject of Research: Automated identification of individuals at high imminent fracture risk
Article Title: Introducing FREMML: a decision-support approach for automated identification of individuals at high imminent fracture risk
Article References:
Rietz, M., Brønd, J.C., Möller, S. et al. Introducing FREMML: a decision-support approach for automated identification of individuals at high imminent fracture risk.
Arch Osteoporos 20, 140 (2025). https://doi.org/10.1007/s11657-025-01613-5
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11657-025-01613-5
Keywords: Fracture risk, FREMML, machine learning, osteoporosis, healthcare innovation.
Tags: advanced decision support systemsaging population health interventionsclinical indicators for bone healthcomprehensive patient data analysisdemographic data in health predictionsfracture risk predictioninnovative fracture risk assessmentlifestyle factors influencing fracturesmachine learning in healthcareosteoporosis management toolsproactive healthcare solutionsRietz Brønd Möller research study