In recent years, the rising prevalence of chronic diseases such as diabetes and hypertension has posed significant challenges to healthcare systems worldwide, especially in developing countries. A comprehensive study conducted by Kocher, Uppal, Purohit, and their team has shed light on the economic implications of managing these illnesses within government healthcare facilities in Punjab, India. Their research, published in BMC Health Services Research, investigates the costs associated with diabetes and hypertension services, offering invaluable insights into systemic barriers and potential avenues for improving health outcomes.
The focus of the study is particularly pertinent as India grapples with an unprecedented surge in non-communicable diseases (NCDs). The World Health Organization has flagged these chronic conditions as crucial public health challenges, and the ramifications of their management extend beyond individual health. With limited resources, the Indian healthcare system strives to meet the demands of a growing population afflicted by these conditions, making this research especially relevant. The findings reflect not only the financial burden on the healthcare system but also underline the need for policy reform and enhanced resource allocation.
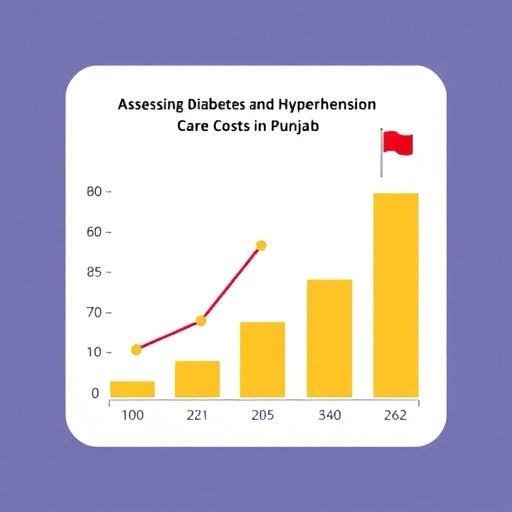
The research team meticulously aimed to quantify the costs incurred by primary and secondary-level government facilities in Punjab when delivering services for diabetes and hypertension. They employed a comprehensive methodology that encompassed both direct and indirect costs associated with patient management. This holistic approach enables a clearer understanding of the true financial burden faced by healthcare providers. By distinguishing between various types of costs, the study provides a nuanced view of economic pressures experienced at different healthcare tiers.
One particularly revealing aspect of the study is the analysis of direct costs, which include expenses for medications, medical supplies, laboratory tests, and personnel involved in patient management. The findings highlight that these direct costs account for a substantial portion of the total expenditure related to treating diabetes and hypertension. With the increasing incidence of these conditions, the financial demands on government facilities are expected to escalate, necessitating urgent attention from health administrators and policymakers.
Further, the research also addressed indirect costs, which encompass lost productivity due to illness and the broader economic impacts on families and communities. The emotional and physical toll of managing chronic diseases cannot be overstated, as patients often find themselves navigating a complex landscape of medical consultations, diagnostic tests, and ongoing treatment regimens. This aspect of chronic disease management not only affects individual patients but also reverberates through their families and communities, straining socio-economic fabrics.
A startling revelation from the study is the disparity in costs between primary and secondary-level government facilities. The results suggest that secondary-level facilities, tasked with more complex cases, bear disproportionately higher costs. This discrepancy underscores the necessity for integrating care at all levels of the health system to ensure that patients receive equitable treatment regardless of the healthcare facility they access. Moreover, it emphasizes the need for strengthening referral systems and enhancing the competence of primary-level facilities.
The researchers also made a compelling case for preventive care as a means to mitigate the escalating costs associated with chronic disease management. By investing in early detection and lifestyle modification initiatives, significant savings could be achieved in the long run. This preventive approach addresses the root causes of diabetes and hypertension while simultaneously improving quality of life for patients. The data suggests that effective community engagement and education around these chronic conditions could alleviate pressures on healthcare resources.
Additionally, the study identified barriers to accessing care within the government health system. Factors such as poor infrastructure, inadequate staffing, and insufficient availability of essential medications were highlighted as significant challenges that hinder effective management of diabetes and hypertension. These obstacles often compel patients to seek care from private providers, further inflating personal expenditure on health services and undermining the efficacy of public health initiatives.
The implications of the study extend beyond the financial realm; they touch upon the broader societal impact of chronic diseases. Diabetes and hypertension are not merely health issues; they represent a socioeconomic concern that can affect productivity and economic growth. As the workforce ages and the prevalence of these diseases continues to rise, the potential for diminished economic output poses a significant challenge for sustainable development in the region.
Furthermore, the researchers underscore the importance of data-driven policy-making in combating the rising tide of NCDs. Policymakers must rely on empirical evidence to allocate resources effectively and design interventions tailored to the needs of different populations. The study serves as a crucial stepping stone in this regard, providing a clear picture of the costs associated with diabetes and hypertension management that can inform future health policies.
In conclusion, the comprehensive research conducted by Kocher and colleagues serves as a vital contribution to the discourse surrounding chronic disease management within the Indian healthcare context. The insights gleaned from their analysis not only reveal the economic burden faced by government facilities in Punjab but also illuminate the critical role of preventive measures and systemic reforms in addressing the rising prevalence of diabetes and hypertension. As policymakers and health administrators reflect on these findings, there is an urgent need to prioritize interventions that enhance accessibility and affordability of care, ultimately improving health outcomes for millions of individuals affected by these chronic conditions.
Subject of Research: Cost of diabetes and hypertension services in Punjab, India.
Article Title: Cost of diabetes and hypertension services delivered in primary and secondary-level government facilities in Punjab, India.
Article References:
Kocher, E.L., Uppal, T., Purohit, N. et al. Cost of diabetes and hypertension services delivered in primary and secondary-level government facilities in Punjab, India.
BMC Health Serv Res (2026). https://doi.org/10.1186/s12913-026-14058-4
Image Credits: AI Generated
DOI:
Keywords: Diabetes, Hypertension, Healthcare Costs, Punjab, India, Non-communicable Diseases.
Tags: BMC Health Services Research findingschronic disease management Indiadiabetes care costs in Punjabeconomic implications of diabetesgovernment healthcare facilities costshealthcare system challenges Punjabhypertension healthcare serviceshypertension treatment expensesnon-communicable diseases public healthpolicy reform for chronic diseasesresource allocation in healthcarerising prevalence of diabetes and hypertension