In the realm of orthopedic surgery, particularly within the scope of meniscal allograft transplantation, significant advancements are being accomplished through the application of patient-specific three-dimensional (3D) modeling. This innovative approach allows for tailored surgical strategies that can enhance patient outcomes and optimize procedural efficiency. Researchers, including Riveros, Quiceno, and Arias Pérez, have explored this intersection of technology and medicine, particularly focusing on the creation of patient-specific tibial models that are revolutionizing surgical planning.
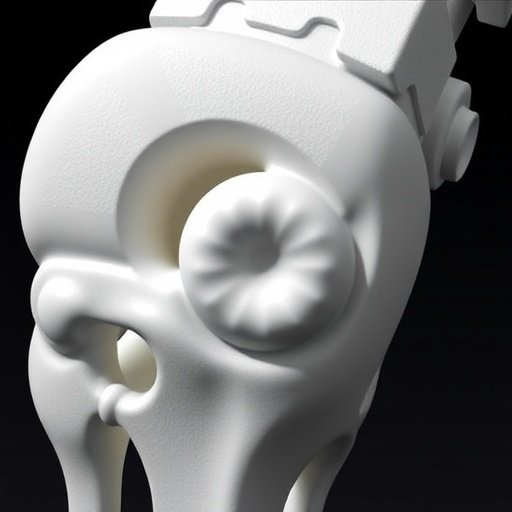
As orthopedic professionals strive to optimize surgical interventions for individuals with meniscal damage, the conventional techniques are met with limitations. Traditional methods often rely on two-dimensional imaging, providing inadequate anatomical detail and limiting surgeons’ understanding of the complex biomechanics at play. However, the introduction of 3D tibial models marks a pivotal advancement, allowing for a more nuanced visualization of the patient’s unique anatomy. By transforming digital imaging data into three-dimensional structures, the surgical team can meticulously analyze the tibia’s morphology, which is crucial for successful allograft preparation and placement.
The advantage of utilizing these patient-specific models transcends mere visualization. Surgeons can simulate surgery, rehearse the procedure, and tailor the surgical plan according to the individual’s anatomical variances. This not only enhances the surgeon’s confidence but also significantly reduces the risk of intraoperative complications, which are often a byproduct of unexpected anatomical challenges during surgery. The enhanced preoperative planning afforded by 3D modeling helps to streamline the surgical process, ultimately benefiting both the surgeon and the patient.
Moreover, the integration of advanced 3D printing technologies into this framework has enabled the creation of tangible physical models. Surgeons can hold and manipulate these models, providing a tactile experience that offers insights unattainable through digital means alone. This hands-on approach can be particularly beneficial in complex cases or when surgical variables are uncertain. Surgeons are able to identify the best strategies for allograft implantation, improving the prospects for successful integration of the graft postoperatively.
The development of these patient-specific models also aligns well with the overarching goals of personalized medicine—a burgeoning field that emphasizes tailored treatment protocols based on individual patient profiles. By utilizing a patient’s unique anatomical characteristics, the surgical approach can be fine-tuned to enhance outcomes, mitigate risks, and facilitate a smoother rehabilitation process. This paradigm shift toward customized surgical interventions is redefining the standards of care in orthopedic surgery.
Furthermore, the implications of this technology extend beyond the operating room. Enhanced preoperative planning through the use of 3D tibial models can lead to reduced operative times, which is a significant contributor to healthcare costs. Shorter surgeries not only minimize exposure to anesthesia but can also lead to a quicker recovery for patients, ultimately benefiting the healthcare system as a whole. By harnessing the power of 3D modeling, hospitals and clinics can potentially see improved resource allocation and enhanced surgery throughput.
As surgical techniques evolve, so must the training of future orthopedic surgeons. Incorporating these advanced technologies into educational curriculums can equip new surgeons with the skills and experience required to navigate increasingly complex procedures. The opportunity to engage with 3D models and simulations during their training will enhance their learning and bolster their confidence when faced with real-life surgical challenges. The pathway to becoming a competent orthopedic surgeon is made richer and more varied with the inclusion of such innovative tools.
In the landscape of orthopedic surgery, the challenge of managing surgical precision continues to grow. The introduction of 3D tibial models in the context of meniscal allograft transplantation signifies a monumental step forward. With ongoing research and advancement, the potential to refine these models exists, leading to further enhancements in their accuracy and applicability. As the technology matures, one can envision a future where every orthopedic intervention is facilitated through 3D modeling, solidifying its place in surgical standard practice.
The road ahead for patient-specific 3D modeling is indeed filled with promise. As clinical applications continue to expand, researchers are anticipated to disseminate findings that underscore the effectiveness and reliability of these model systems. Future studies will be pivotal, building on existing knowledge while exploring the interplay between various orthopedic conditions and patient-specific modeling techniques. This continuous quest for innovation serves as a reminder of the transformative capabilities of technology in improving human health.
Ultimately, as healthcare moves toward an era characterized by integration of sophisticated technological solutions into everyday practices, patient-specific 3D modeling stands at the forefront of orthopedic advancements. The evolution of surgical techniques through this innovative approach illustrates a harmonious blend of medicine and technology in addressing the needs of patients. As this research progresses, it invariably lays the groundwork for a future where surgical precision and individualized care are seamlessly intertwined.
This wave of change not only impacts surgical practice but also enhances patient education and engagement. Armed with a physical model of their anatomy, patients are empowered to participate actively in their care decisions. Observing how their unique structures are considered during the planning of their surgeries fosters a stronger clinician-patient relationship. Empowering patients through education represents a critical component in the healthcare equation, and these advancements in modeling are driving a more informed patient population.
As new surgical methods continue to emerge, the community of orthopedic surgeons eagerly anticipates the next phase of patient-specific application. The potential for further integration of artificial intelligence and machine learning will likely augment the development of these models, increasing their predictive capabilities and precision. The quest for personalization in treatment approaches remains a cornerstone in orthopedic medicine, and the integration of advanced modeling truly signifies a leap toward achieving that goal.
Research efforts such as those conducted by Riveros and colleagues serve as an inspiring testament to the transformative impact of technology in medicine. The profound implications of their work extend far beyond the walls of research institutions and operating rooms; they resonate deeply within the patient community, offering renewed hope and direction for those affected by meniscal injuries. In conclusion, the field of orthopedic surgery stands at an exciting brink, where patient-specific 3D tibial modeling is paving the way for a revolutionary transformation in surgical care and patient outcomes.
Subject of Research: Patient-specific 3D tibial models in meniscal allograft transplantation
Article Title: Patient-specific 3D tibial model: transforming meniscal allograft transplantation and surgical planning
Article References: Riveros, P.A.S., Quiceno, A.J. & Arias Pérez, R. Patient-specific 3D tibial model: transforming meniscal allograft transplantation and surgical planning. 3D Print Med 11, 20 (2025). https://doi.org/10.1186/s41205-025-00267-w
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s41205-025-00267-w
Keywords: 3D modeling, meniscal allograft, orthopedic surgery, personalized medicine, surgical planning