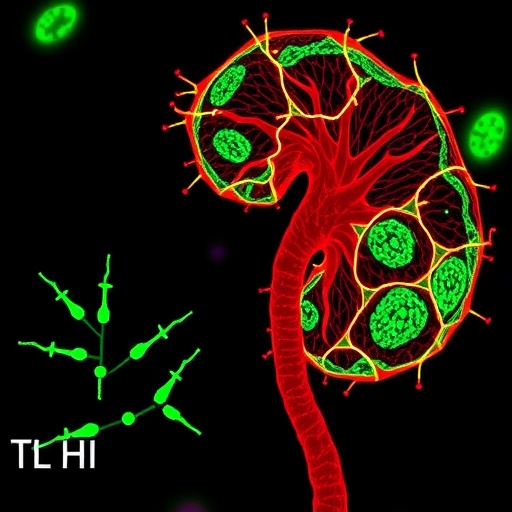
A significant body of research has revealed critical insights into the intricate world of autoimmune disorders in children, providing a detailed examination of pediatric-onset anti-contactin1 antibody-associated autoimmune nodopathies, particularly when these conditions exist alongside membranous nephropathy. Researchers have identified this unique intersection, highlighting how one autoimmune condition can impact the progression and severity of another. This revelation opens new avenues for understanding the pathophysiology of autoimmune diseases in the pediatric population.
Autoimmune disorders are characterized by a body’s immune system mistakenly targeting its own tissues. Understanding the triggers and manifestations of these conditions in children is particularly challenging, as immune responses can vary significantly compared to adults. The focus of the latest study sheds light on anti-contactin1 antibodies, which are known to be involved in various neurological and autoimmune conditions. In this new research, the authors provide a comprehensive evaluation of the clinical features exhibited by affected pediatric patients, adding substantial value to existing literature.
The research journey began with a thorough review of clinical cases involving children presenting symptoms of autoimmune nodopathies. Sensory and motor dysfunctions were prevalent among these patients, prompting investigators to delve deeper into the autoimmune mechanisms at play. The researchers meticulously gathered data on the symptoms, laboratory findings, and treatment responses of these children, offering a holistic view of their health challenges. This approach aims to characterize the differences and commonalities among pediatric patients suffering from similar autoimmune disorders.
One of the standout findings of this research is the observed prevalence of membranous nephropathy in conjunction with anti-contactin1 antibody-associated nodopathies. Traditionally, membranous nephropathy has been viewed as an isolated renal condition; however, this study suggests a potential autoimmune link that requires further exploration. The presence of both disorders in the same patient cohort raises significant questions regarding their interrelation and the potential shared pathophysiological mechanisms.
In the context of pediatric nephrology, understanding the implications of co-existing autoimmune conditions is paramount. The findings underline the necessity for clinicians to adopt a more integrative approach when diagnosing and managing pediatric autoimmune disorders. This broader perspective may facilitate early detection of concomitant conditions, ultimately improving patient outcomes. The integration of nephrology and immunology practices may allow for tailored treatment approaches that can address both the neurological and renal aspects of patient health.
The implications of this research extend beyond the clinical realm, fostering a deeper understanding of immune dysregulation in pediatric patients. As studies continue to reveal the complexities of autoimmune disorders, there is a growing recognition of the need for multidisciplinary collaborations. By uniting experts from various medical fields, a more comprehensive grasp of these conditions can be achieved, leading to advancements in both research and treatment methodologies.
Additionally, the study emphasizes the importance of genetic factors in the predisposition to autoimmune disorders. Investigators have observed that familial occurrences of anti-contactin1 antibodies may suggest a hereditary component to these diseases. Further genetic analyses aim to illuminate the underlying genetic correlations, with the hope of identifying biomarkers that could aid in predicting susceptibility.
While the findings of this study are undoubtedly groundbreaking, they also pose a myriad of questions that warrant further investigation. The researchers speculate about the underlying immunological triggers for the simultaneous occurrence of autoantibodies and renal involvement. Environmental factors, infections, and even lifestyle changes could contribute to the onset of these autoimmune responses in susceptible children.
Looking toward future research, it is essential that questions around the age of onset, the duration of symptoms, and response to immunotherapy are addressed. The response of pediatric patients to existing therapeutic protocols feels urgent in the light of this study’s findings. New targeted therapies can potentially emerge from understanding the distinct autoimmune profiles of affected children, ultimately leading to more personalized care strategies that can better manage the disease.
Importantly, the collaborative nature of this research provides a framework for future studies exploring other antibody-associated conditions in children. The insights gleaned from evaluating the relationship between anti-contactin1 antibodies and kidney function could very well extend to other autoimmune conditions, paving the way for a broader understanding of the pediatric autoimmune landscape.
As the medical community processes this information, it raises critical discussions on the significance of timely and accurate diagnosis in the realm of pediatric autoimmune disorders. Ultimately, this study advocates for raising awareness among healthcare providers regarding concomitant autoimmune conditions and their potential impact on treatment strategies. Knowledge-sharing amongst practitioners will undoubtedly play a pivotal role in enhancing patient care in this niche field of medicine.
In conclusion, the exploration of pediatric-onset anti-contactin1 antibody-associated autoimmune nodopathies in conjunction with membranous nephropathy underscores the evolving understanding of autoimmune diseases. This study is essential for shaping future research directions, improving diagnostic protocols, and refining therapeutic strategies for children grappling with these complex health issues.
Subject of Research: Pediatric-onset anti-contactin1 antibody-associated autoimmune nodopathies and membranous nephropathy.
Article Title: Characteristics of pediatric-onset anti-contactin1 antibody-associated autoimmune nodopathies with concomitant membranous nephropathy.
Article References:
Guan, Q., Xie, Y., He, Y. et al. Characteristics of pediatric-onset anti-contactin1 antibody-associated autoimmune nodopathies with concomitant membranous nephropathy. BMC Pediatr (2026). https://doi.org/10.1186/s12887-025-06429-3
Image Credits: AI Generated
DOI:
Keywords: Autoimmune Disorders, Pediatric Health, Anti-Contactin1 Antibodies, Membranous Nephropathy, Immune Dysregulation.
Tags: anti-contactin1 antibodiesautoimmune disease progression in childrenautoimmune disease triggers in childrenautoimmune nodopathies in pediatricsimmune system dysfunction in childrenmembranous nephropathy in childrenneurological autoimmune conditionspathophysiology of autoimmune diseasespediatric autoimmune disorderspediatric clinical case studiespediatric nephrology researchsensory motor dysfunction in pediatric patients