In a groundbreaking study published in the Journal of Translational Medicine, researchers have unveiled a novel method for diagnosing chronic fatigue syndrome (CFS) through the utilization of beat-to-beat autonomic measurements. This innovative approach holds promise for more accurate and efficient identification of CFS, a condition characterized by profound fatigue and an array of debilitating symptoms that traditionally eluded precise diagnostic criteria.
Chronic fatigue syndrome has long been a perplexing ailment, affecting millions worldwide yet lacking a universally accepted diagnostic marker. Symptoms often manifest as persistent exhaustion, cognitive difficulties, and unrefreshing sleep, leading to a significant decline in the quality of life for those affected. Conventional diagnostic methods have primarily relied on subjective patient reports and exclusionary criteria, often leaving many without a proper diagnosis. This study offers new hope by integrating advanced physiological measurements into the diagnostic process.
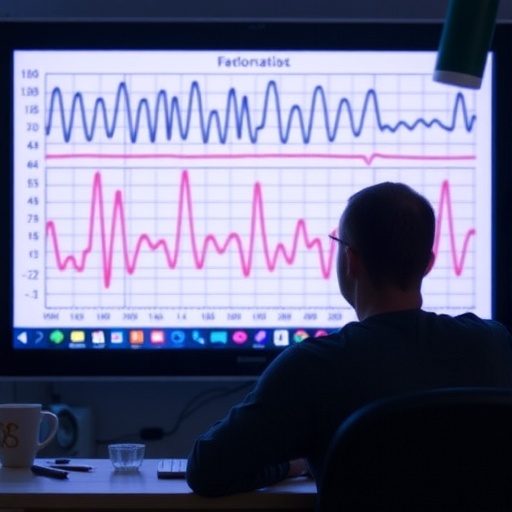
The researchers, led by S. Kujawski and H. Tabisz, combined state-of-the-art autonomic function tests with thorough clinical evaluations to distinguish patients suffering from CFS from healthy individuals. Their work harnesses the power of continuous heart rate variability and blood pressure monitoring—two critical indicators of autonomic nervous system function that can provide insights into the underlying pathophysiology of fatigue syndromes.
Central to the study’s success was the use of beat-to-beat measurements, which allow for a more granular analysis of cardiovascular responses in real-time. This fine-tuned approach stands in stark contrast to traditional, less sensitive methods of cardiovascular assessment, which may miss subtle changes in autonomic regulation. By focusing on the intricate dynamics of heart rate and blood pressure fluctuations, the team aimed to uncover patterns uniquely associated with CFS.
The research further explores the relationship between autonomic function and fatigue. Autonomic dysregulation has been implicated in CFS, and the team’s findings bolster this connection. Their analysis revealed distinct heart rate variability profiles among CFS patients that are markedly different from those in healthy controls. These profiles may serve as biomarkers for the condition, offering a potential pathway for clinicians to diagnose and understand CFS more clearly.
Throughout the study, the emphasis was placed on robust data collection and analysis. By employing a combination of advanced statistical techniques and machine learning algorithms, researchers were able to sift through vast amounts of physiological data to identify key indicators associated with chronic fatigue. This data-driven approach not only enhances the reliability of the diagnosis but also aligns with contemporary moves towards precision medicine, where treatments are tailored based on individual patient profiles.
Furthermore, the implications of this research extend beyond diagnosis; they hint at potential therapeutic targets. Understanding the specific autonomic disturbances in CFS could pave the way for new treatment modalities that address the root causes of the syndrome, rather than merely alleviating symptoms. Enhancements in patient management are within reach if clinicians can accurately diagnose based on these physiological metrics.
The findings from Kujawski et al. also raise important questions about the nature of CFS itself. The evidence points towards a multifaceted disorder, possibly linked to viral infections or autoimmune responses that disrupt normal autonomic function. As the study gains traction within the scientific community, it may stimulate further research aimed at elucidating the complex interactions between infections, immune system responses, and neurologic symptoms.
Moreover, this emphasis on empirical measurement represents a critical shift in how CFS is perceived within both medical and patient communities. Historically, CFS was often stygmatized, leading to skepticism about its legitimacy as a medical condition. By establishing a physiological basis for diagnosis, the research advocates for an enhanced recognition of CFS as a legitimate illness deserving of medical attention and research funding.
The study contributes to a growing body of literature indicating that many chronic illnesses exhibit underlying autonomic dysfunction. In this context, the investigative efforts could foster new collaborations across disciplines, uniting researchers in neurology, immunology, and cardiology in a quest to untangle the biological underpinnings of these complex syndromes.
The extensive participant cohort in the study enhances the generalizability of the findings, ensuring that the results offer insights applicable to diverse populations. The authors acknowledge the necessity of further studies to validate these findings across different demographics and clinical settings, highlighting the importance of inclusivity in biomedical research.
In summary, the innovative approach to diagnosing chronic fatigue syndrome revealed in this study exemplifies a pivotal moment in understanding a previously nebulous ailment. By anchoring the diagnosis in quantifiable autonomic measurements, this work promises to transform clinical practices and improve the lives of individuals impacted by CFS. As the pursuit of deeper understanding continues, it becomes ever clearer that the intersection of technology and medicine holds the key to unlocking the mysteries surrounding chronic fatigue and similar disorders.
As the scientific community delves further into the implications of these findings, it is expected that new lines of inquiry will emerge, each building on the foundation laid by Kujawski and his colleagues. The integration of innovative diagnostic methodologies not only heralds a new chapter for chronic fatigue syndrome but also sets a precedent for the future of disease diagnosis and management.
In conclusion, the journey towards establishing a cohesive and validated framework for chronic fatigue syndrome diagnosis is only just beginning. The collaborative efforts of researchers, clinicians, and patients alike will be crucial as we strive for a better understanding of this complicated condition. Through innovation, thorough research, and clinical application, the paradigm surrounding chronic fatigue may be fundamentally transformed, bringing much-needed hope to those affected by this syndrome.
Subject of Research: Diagnosis of chronic fatigue syndrome using beat-to-beat autonomic measurements.
Article Title: Diagnosis of chronic fatigue syndrome using beat-to-beat autonomic measurements.
Article References: Kujawski, S., Tabisz, H., Morten, K.J. et al. Diagnosis of chronic fatigue syndrome using beat-to-beat autonomic measurements. J Transl Med 23, 1413 (2025). https://doi.org/10.1186/s12967-025-07433-y
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12967-025-07433-y
Keywords: Chronic fatigue syndrome, autonomic measurements, heart rate variability, diagnosis, translational medicine.
Tags: advancements in chronic illness diagnosisautonomic measurement techniquesblood pressure monitoring in CFSchronic fatigue syndrome diagnosisdistinguishing CFS from healthy individualsH. Tabisz clinical evaluationheart rate variability analysisimpact of CFS on quality of lifeinnovative diagnostic methods for fatiguepathophysiology of fatigue syndromesphysiological indicators of chronic fatigueS. Kujawski research study