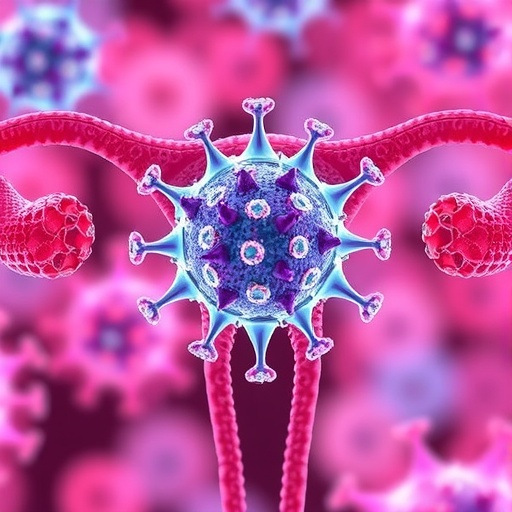
Recent scientific findings have illuminated the intricate relationship between human papillomavirus (HPV) and ovarian cancer, particularly focusing on the inflammatory pathways that the virus manipulates to foster carcinogenesis. A pivotal study conducted by Kermanshahi et al. reveals how HPV can play a significant role in altering the immune response, thereby creating an environment conducive to the development of ovarian cancer. These revelations emphasize the need for a deeper investigation into how viral infections contribute to cancer progression and underline the potential for targeted therapies.
The research team meticulously examined how HPV interacts with the host’s biological systems, specifically targeting key molecular pathways involved in inflammation. This inquiry is of paramount importance as inflammation is now recognized as a critical factor in cancer development. The immune response triggered by HPV infection might initially aim to eliminate the virus, yet it paradoxically creates a microenvironment that promotes tumor growth. The findings raise crucial questions about the dual nature of this immune response, suggesting that the very mechanisms designed to protect us could inadvertently facilitate oncogenesis.
Among the intricate mechanisms at play, the study highlights the role of cytokines and chemokines. These signaling proteins are crucial for mediating the immune response but can also enhance tumor growth when produced in excess or inappropriately. The research provides compelling evidence that HPV infection can lead to dysregulation of these inflammatory signals, fostering a pro-tumorigenic environment. This dysregulation might not only promote cell proliferation but also aid in escaping apoptosis, allowing damaged cells to survive and proliferate uncontrollably.
In addition to elucidating the molecular mechanisms, Kermanshahi et al. underscore the therapeutic implications of their findings. As our understanding of the role of HPV in ovarian cancer deepens, it opens up new avenues for treatment strategies. The researchers propose that targeting the inflammatory pathways exacerbated by HPV might offer a novel approach for therapeutic intervention. This could involve the use of anti-inflammatory agents or therapies designed to re-establish a balanced immune response, potentially curbing the progression of the disease.
The study also brings attention to the importance of early detection and prevention strategies directed toward HPV-related malignancies. As HPV is a preventable cause of several cancers, increasing vaccination efforts and screening could significantly reduce the incidence of these tumors. The research advocates for integrating HPV vaccination programs into public health initiatives, particularly targeting populations at risk for ovarian and other HPV-related cancers to mitigate the long-term effects of the virus.
Moreover, the collaboration among various disciplines in this research signifies a shift towards a more holistic understanding of cancer biology. By uniting virology, immunology, and oncology, the study exemplifies how interdisciplinary approaches can unveil complex relationships within cancer pathogenesis. This collaboration is critical, not only for advancing our scientific knowledge but also for fostering innovative therapeutic strategies that could transform clinical outcomes for patients.
The potential prospect of utilizing personalized medicine based on the molecular mechanisms elucidated by the research cannot be overlooked. Understanding the specific role of HPV in ovarian carcinogenesis could lead to the development of targeted therapies that align with the unique tumor microenvironment of individual patients. Such precision medicine approaches could vastly improve treatment efficacy and minimize unwanted side effects associated with conventional therapies.
This groundbreaking study advocates for further research into the various strains of HPV and their differential roles in the pathogenesis of ovarian cancer. It sparks a new line of inquiry into how genetic variations of the virus might influence the inflammatory response and, consequently, cancer development. This dimension of research could significantly enhance our understanding of how specific HPV types correlate with different cancer phenotypes, potentially leading to more tailored prevention strategies.
The implications of Kermanshahi et al.’s work extend beyond the immediate scope of ovarian cancer. As we grapple with the burden of cancer globally, understanding viral contributions to malignancies poses an urgent need to develop efficient prevention and treatment strategies. The insights from their research could potentially be applicable to other HPV-associated cancers, encouraging a broader investigation into antiviral strategies that could help combat various oncological challenges.
Despite the promising results, the study does not shy away from highlighting the limitations of current research. There is an urgent need for more comprehensive studies involving larger patient cohorts to validate the proposed mechanisms and therapeutic interventions. Additionally, exploring the interplay of HPV with other environmental carcinogens will provide a clearer picture of multifactorial carcinogenesis and may yield further targets for therapeutic intervention.
As complementary research emerges, the prospect of translational applications grows increasingly viable. With ongoing advancements in molecular biology and immunotherapy, the field of oncology is poised for rapid evolution. The clarion call to innovate and employ novel strategies to combat HPV-driven cancers resonates strongly, providing a renewed sense of urgency for researchers and clinicians alike.
The narrative of HPV in the context of ovarian cancer continues to unfold, and with this research, a clearer picture of its profound impact on inflammatory pathways is emerging. Through dedicated efforts in research and public health, we can aspire to reduce the burden of HPV-related cancers, transforming the landscape of oncological care in the years to come.
The unfolding understanding of the interplay between viral oncogenesis and inflammation highlights the intricate complexity of cancer biology. As research progresses, the medical community remains steadfastly focused on unraveling these enigmas, with the ultimate goal of improving patient outcomes and eradicating the scourge of cancer on a global scale.
Subject of Research: HPV and its role in ovarian carcinogenesis through inflammatory pathways.
Article Title: HPV-driven inflammatory pathways in ovarian carcinogenesis: molecular mechanisms and emerging therapeutic interventions.
Article References:
Kermanshahi, A.Z., Ebrahimi, F., Taherpoor, A. et al. HPV-driven inflammatory pathways in ovarian carcinogenesis: molecular mechanisms and emerging therapeutic interventions.
J Ovarian Res (2025). https://doi.org/10.1186/s13048-025-01948-0
Image Credits: AI Generated
DOI: 10.1186/s13048-025-01948-0
Keywords: HPV, ovarian cancer, inflammatory pathways, oncogenesis, therapeutic interventions.
Tags: cytokines and chemokines in cancerdual nature of immune response in cancerHPV and ovarian cancer relationshipimmune response to HPV infectionimplications of HPV in women’s healthinflammatory pathways in cancer developmentmechanisms of HPV-induced carcinogenesisresearch on HPV and ovarian cancerrole of inflammation in tumor growthtargeted therapies for HPV-related cancersunderstanding cancer microenvironments.viral infections and cancer progression