In a groundbreaking study published in Pediatric Research on December 3, 2025, researchers have unveiled critical insights into the long-term musculoskeletal and pulmonary outcomes of adults who underwent open esophageal atresia repair during infancy. Employing an innovative imaging technique—real-time magnetic resonance imaging (MRI)—the research team has transcended traditional diagnostic boundaries to provide a dynamic, comprehensive understanding of how early surgical intervention influences bodily function decades later.
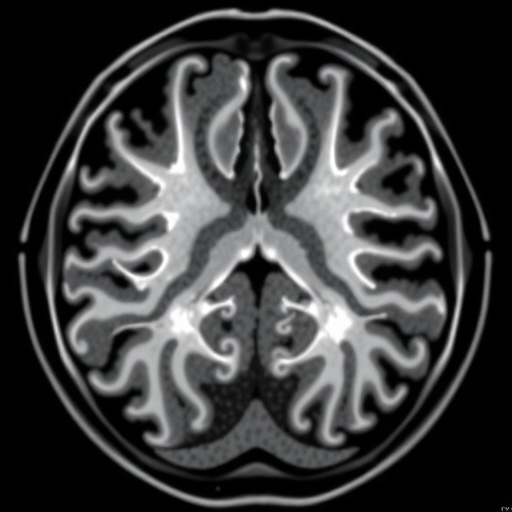
Esophageal atresia, a congenital defect characterized by the discontinuity of the esophagus, often necessitates prompt surgical correction shortly after birth to restore gastrointestinal continuity. While the immediate postoperative outcomes have been extensively documented, the enduring effects of this complex reconstruction—particularly on respiratory mechanics and thoracic musculoskeletal integrity—have remained elusive. By leveraging real-time MRI, the present investigation offers an unparalleled portrayal of respiratory dynamics correlated with structural and functional musculoskeletal adaptations in adult patients who underwent this surgery in childhood.
The study cohort comprised adults who, as neonates, received open esophageal atresia repair. Over the past years, these individuals have faced variable respiratory challenges, yet conventional static imaging and pulmonary function tests have failed to elucidate the nuanced interplay between lung capacity fluctuations and muscular skeletal constraints. Real-time MRI techniques overcame these limitations by capturing live respiratory motion, allowing assessment not only of static anatomical abnormalities but also of dynamic airway behavior and chest wall kinetics throughout the breathing cycle.
Importantly, the imaging sequences used were tailored to visualize high-temporal-resolution thoracic anatomy without ionizing radiation, thus providing a safe method suitable for longitudinal follow-up studies. The researchers meticulously quantified parameters such as diaphragm excursion, rib cage expansion, and ventilatory patterns during different respiratory phases. This approach shed light on the compensatory mechanisms elicited by residual structural irregularities and provided compelling evidence that esophageal atresia repair has lasting ramifications extending beyond the initial anatomical correction.
Findings revealed distinctive alterations in chest wall mechanics, particularly decreased thoracic compliance and altered rib cage motion, which were correlated with diminished pulmonary function test outcomes. These adaptations often result in restricted lung volumes and may predispose individuals to chronic respiratory complications, including reduced exercise tolerance and susceptibility to respiratory infections. Furthermore, the study revealed a tendency for thoracic musculoskeletal remodeling, likely a consequence of altered biomechanical loading, as the body adapts to the congenital and surgical constraints.
One of the more surprising outcomes of the investigation was the revelation that even in the absence of overt clinical symptoms, subtle functional impairments could be detected by real-time MRI—highlighting its sensitivity and potential as a prognostic tool. These subclinical presentations could have been easily overlooked with standard diagnostic methods, underscoring the importance of advanced imaging in the comprehensive evaluation of this unique patient population.
Additionally, the study contextualized its findings within a broader framework of pediatric surgical follow-up protocols. Current practice often neglects long-term musculoskeletal assessments, focusing predominantly on gastrointestinal and respiratory symptomatology alone. These new insights advocate for a multidisciplinary approach that incorporates routine, dynamic imaging assessments to better anticipate and manage potential sequelae.
Beyond the technical and clinical revelations, the research embodies a paradigm shift in understanding how early life surgical interventions yield biomechanical ripple effects that persist well into adulthood. The interplay between repaired anatomical structures and compensatory musculoskeletal changes constitutes a complex, evolving system that demands vigilant monitoring and tailored therapeutic strategies.
The implications for rehabilitation medicine are profound. Data indicating impaired thoracic mobility suggest that targeted physical therapy regimens focusing on chest wall flexibility and respiratory muscle strengthening may ameliorate functional deficits and enhance quality of life. Early identification of patients at risk through real-time MRI could personalize interventions, potentially reducing long-term morbidity.
Moreover, this technique holds promise for expanding the horizons of respiratory research beyond esophageal atresia. Real-time MRI’s ability to capture dynamic physiologic processes invites applications in diverse pulmonary and musculoskeletal disorders where functionally relevant morphological changes elude detection through static imaging.
From a surgical perspective, understanding the biomechanical consequences of the repair method could inspire refinements in operative techniques aimed at minimizing adverse long-term effects. Surgeons might adjust reconstructive approaches to preserve thoracic compliance or employ adjunctive measures to support musculoskeletal integrity from the outset.
The integration of cutting-edge imaging technology with clinical follow-up in this study exemplifies how translational research can refine not only our understanding but also the care paradigms for congenital anomalies. It underscores the importance of viewing pediatric surgical outcomes through a life-course lens to optimize health trajectories and functional resilience.
As the cohort ages, future investigations will be crucial to delineate the progression of musculoskeletal and pulmonary alterations and to quantify their impact on morbidity and mortality. Longitudinal studies incorporating real-time MRI could illuminate the natural history of these adaptations and guide evidence-based interventions.
Ultimately, this investigation into open esophageal atresia repair survivors redefines the scope of postoperative assessment and heralds a new era in personalized medicine for congenital disorder management. By illuminating unseen facets of respiratory and musculoskeletal interaction, it paves the way for enhanced diagnostic precision, optimized therapies, and improved long-term health outcomes.
The marriage of precision imaging and clinical expertise demonstrated in this study underscores the transformative potential of contemporary biomedical research to deliver insights that reverberate from microscopic physiological insights to macroscopic patient well-being.
Subject of Research: Long-term musculoskeletal and pulmonary outcomes in adults following open esophageal atresia repair.
Article Title: Adults following open esophageal atresia repair: evaluating long-term musculoskeletal and pulmonary outcomes using insights from real-time MRI.
Article References:
Aubert, O., Lacher, M., Frahm, J. et al. Adults following open esophageal atresia repair: evaluating long-term musculoskeletal and pulmonary outcomes using insights from real-time MRI. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04568-y
Image Credits: AI Generated
DOI: 03 December 2025
Tags: adult health after esophageal atresia repaircongenital esophageal defects researchdynamic MRI for respiratory assessmentesophageal atresia and thoracic integrityinnovative imaging techniques in pediatric surgerylong-term follow-up of surgical interventionslong-term outcomes of esophageal atresiamusculoskeletal effects of esophageal atresia surgerypediatric surgery outcomes in adulthoodpulmonary function in adults with congenital defectsreal-time MRI in medical researchrespiratory dynamics in post-surgical patients