In a groundbreaking advancement poised to revolutionize the management and treatment of Parkinson’s disease, researchers have unveiled a novel nanoMolecularly Imprinted Polymer (nanoMIP) sensor capable of monitoring levodopa pharmacokinetics in real time within living organisms. This cutting-edge technology promises to usher in a new era of precision medicine, offering unprecedented insights into drug dynamics and individualized therapy optimization for patients battling this debilitating neurological disorder. The study, published in Nature Communications, marks a significant leap forward in bio-sensing and personalized therapeutic monitoring.
Parkinson’s disease is a neurodegenerative condition characterized by the progressive loss of dopamine-producing neurons, leading to motor dysfunction and a range of non-motor symptoms. Levodopa remains the cornerstone of symptomatic treatment, functioning as a dopamine precursor. However, the pharmacokinetics of levodopa—how it is absorbed, distributed, metabolized, and eliminated—vary significantly among patients, complicating dosage optimization. Traditional therapeutic drug monitoring methods rely on periodic blood sampling and clinical assessments, which lack temporal resolution and are often impractical for real-time adjustment.
The novel nanoMIP sensor technology directly addresses these limitations by enabling continuous in vivo monitoring of levodopa concentration in the bloodstream through a minimally invasive implantable platform. NanoMIPs are synthetic polymeric receptors engineered at the nanoscale to possess highly selective binding pockets molded against the target molecule—in this case, levodopa. This molecular imprinting technique confers remarkable specificity and affinity akin to natural antibodies but with superior stability, reproducibility, and cost-effectiveness.
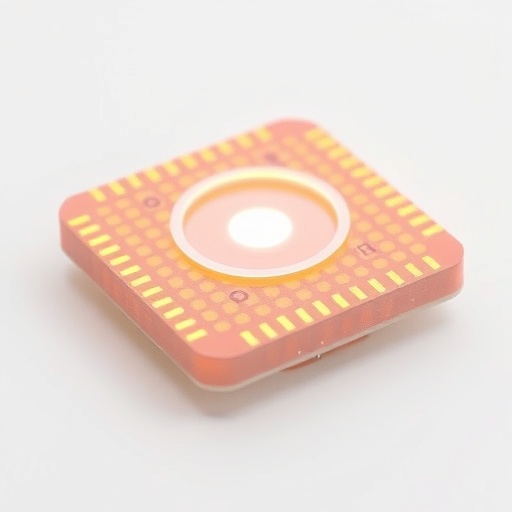
Fabricated through a meticulous process of polymerization in the presence of levodopa templates, the nanoMIPs form uniform nanostructured recognition sites perfectly complementary in size, shape, and functional group orientation to levodopa molecules. Once implanted subcutaneously or integrated into a microfluidic device for in vivo application, the sensor exhibits rapid and reversible binding kinetics, enabling dynamic tracking of fluctuating levodopa levels continuously over extended periods.
Integration of this sensor into a bioelectronic interface allows for transduction of the molecular recognition event into an electrical signal measurable in real time. The researchers engineered a delicate electrochemical sensing platform whereby nanoMIP-coated electrodes exploit changes in impedance or current flow as levodopa binds, generating a quantifiable and highly sensitive readout. This real-time data stream can be wirelessly transmitted to clinicians or wearable devices, facilitating immediate therapeutic adjustments customized to individual pharmacokinetic profiles.
Critically, the sensor demonstrated extraordinary selectivity amid complex biological fluids, effectively distinguishing levodopa from structural analogs and endogenous interfering substances. In vivo experiments conducted on rodent models of Parkinson’s disease revealed that the nanoMIP sensor could continuously monitor levodopa plasma concentrations with exceptional accuracy and temporal resolution. These findings were validated against gold-standard chromatographic assays, confirming the sensor’s reliability and potential utility in a clinical setting.
The ability to monitor levodopa levels continuously transforms the therapeutic landscape, potentially minimizing the risk of motor fluctuations, dyskinesias, and other adverse effects stemming from suboptimal dosing. By providing real-time pharmacokinetic data, the technology enables a feedback loop for closed-loop drug delivery systems or informed clinical decision-making, propelling personalized Parkinson’s care forward.
Beyond Parkinson’s disease, the versatile nanoMIP sensing strategy holds promise across various domains of pharmacology and diagnostics. The modular design allows customization for numerous other biomolecules, drugs, or metabolites, thus broadening its impact to personalized medicine and remote health monitoring across multiple conditions. The robustness of synthetic nanoMIPs circumvents many limitations associated with biological receptors that can deteriorate under physiological conditions.
However, several challenges remain on the pathway to clinical translation. Long-term biocompatibility, sensor fouling in vivo, integration with wearable electronics, and regulatory hurdles must be systematically addressed. The researchers foresee advances in polymer chemistry, microfabrication, and wireless communication technologies will catalyze overcoming these barriers, heralding an era of seamless continuous health monitoring.
The nanoMIP sensor represents an extraordinary fusion of chemistry, nanotechnology, and bioengineering, capturing the zeitgeist of precision healthcare. By shifting therapeutic monitoring from snapshot measurements to real-time molecular tracking, it empowers clinicians with tools to tailor interventions literally minute by minute. Such innovations exemplify how convergence science is reshaping treatment paradigms in chronic diseases like Parkinson’s, dramatically improving patient outcomes and quality of life.
This breakthrough coincides with the global surge in interest around wearable and implantable biosensors, offering complementary capabilities to genetic profiling and biomarker discovery. As the population ages and neurodegenerative diseases rise sharply, scalable solutions for responsive and adaptive therapy become imperative. The nanoMIP sensor stands at this critical juncture, translating molecular insight into actionable control of drug therapy.
Envisioned future implementations might include smart therapeutics where drug delivery pumps communicate bidirectionally with nano-sensors to titrate dosing autonomously. Such closed-loop systems could maintain therapeutic drug levels within optimal windows consistently, mitigating side effects and enhancing effectiveness. The technology also paves the way for large-scale pharmacokinetic studies in real-world settings, providing a richer understanding of interindividual variability and environmental influences on drug response.
In essence, this pioneering research underscores a pivotal leap toward truly personalized Parkinson’s disease management—combining high-precision molecular detection with real-time actionable intelligence. It exemplifies how innovative nanoengineering solutions can overcome longstanding clinical challenges and transform patient care profoundly. As these nanoMIP sensors move closer to human trials, there is renewed hope for Parkinson’s patients who seek better symptom control, fewer complications, and greater independence in daily living.
This remarkable innovation sets a new paradigm, signaling the dawn of a new age in neuropharmacology and wearable biosensing technology. It affirms the power of molecular imprinting at the nanoscale to unlock transformative diagnostic and therapeutic potential. The implications extend beyond a single drug or disease, charting the course for next-generation smart medical devices that integrate seamlessly with the human body’s intricate biochemical networks.
Undoubtedly, this work by Zhou, Li, Xu and colleagues will inspire a wave of research at the interface of polymer chemistry, sensor technology, and neuroscience. It highlights the critical role of interdisciplinary collaboration in addressing complex biomedical challenges. With continued refinement and clinical validation, the nanoMIP sensor could become an indispensable tool in precision pharmacotherapy—ushering in a future where real-time molecular data guides tailored treatments, improves patient safety, and enhances the efficacy of medicines for Parkinson’s and beyond.
Article References:
Zhou, Y., Li, J., Xu, Z. et al. A nanoMIP sensor for real-time in vivo monitoring of levodopa pharmacokinetics in precision Parkinson’s therapy. Nat Commun 16, 10796 (2025). https://doi.org/10.1038/s41467-025-65853-2
DOI: https://doi.org/10.1038/s41467-025-65853-2
Image Credits: AI Generated
Tags: bio-sensing innovations in healthcarecontinuous drug monitoring solutionsdopamine precursor therapyimplantable sensor devicesminimally invasive biosensorsnanoMIP sensor technologyNature Communications research findingsParkinson’s disease treatment advancementspersonalized medicine for neurodegenerative disorderspharmacokinetics of levodopareal-time levodopa monitoringtherapeutic drug optimization methods