The future of muscle assessment in older adults has become an area of increasing interest in medical research, especially given the rising prevalence of sarcopenia—a condition characterized by the loss of muscle mass and function. In a recent commentary, researchers Perkisas, Welch, and Soulis delve into the complexities surrounding muscle ultrasound technology and its role in evaluating sarcopenia. As the aging population continues to grow, understanding the tools available for diagnosing and monitoring muscle health is essential.
Sarcopenia is often a hidden condition that develops gradually, leading to significant health impairments before it becomes clinically apparent. It can result in severe consequences, including increased risk of falls, frailty, and even mortality among older adults. With its silent progression, the challenge lies in early identification and appropriate intervention to improve outcomes for this vulnerable population. This is where medical imaging technologies, such as ultrasound, come into play.
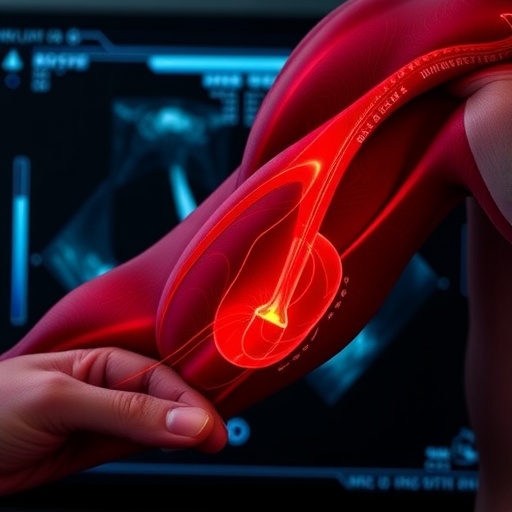
Ultrasound has gained popularity due to its non-invasive nature and ability to provide real-time images of muscle tissue. Unlike traditional imaging modalities like CT scans or MRIs, ultrasound offers a portable and cost-effective solution that can be performed at the bedside. These qualities make it particularly appealing for geriatric patients who often face mobility issues. However, despite its advantages, there remains a skepticism surrounding the reliability and predictive value of ultrasound in accurately diagnosing sarcopenia.
The authors argue that while ultrasound can visualize muscle architecture and assess cross-sectional area, its limitations must also be acknowledged. For example, factors such as hydration status, muscle quality, and the experience level of the operator can significantly affect results. This variability raises questions about the standardization of ultrasound techniques and the establishment of normative data across diverse populations. Until these standards are met, the effectiveness of ultrasound as a diagnostic tool remains uncertain.
Moreover, the debate continues about the most appropriate imaging techniques to complement clinical assessments. While ultrasound holds promise, it may not provide a comprehensive view of muscle functionality. Other methodologies, such as bioelectrical impedance analysis and dual-energy X-ray absorptiometry, offer different insights into body composition. Contextualizing ultrasound within a broader framework of muscle health assessments could provide a more holistic understanding of sarcopenia.
Researchers also emphasize the importance of longitudinal studies to monitor muscle changes over time. Such studies could help delineate the precise role ultrasound might play in tracking the progression of sarcopenia and evaluating the effectiveness of interventions aimed at preserving muscle function. However, large-scale studies specifically targeting ultrasound’s capabilities are still lacking. This gap in research presents an urgent need for studies that bridge the divide between clinical practice and technological innovation.
As the science of muscle aging evolves, interdisciplinary collaboration between geriatricians, radiologists, and biomedical engineers will be critical. The fusion of expertise from diverse fields could lead to the development of enhanced ultrasound technologies that provide more accurate and actionable data on muscle health. Additionally, integrating artificial intelligence into image analysis can further refine our understanding by identifying subtle changes that are often overlooked by traditional assessment tools.
While discussions continue regarding the feasibility of muscle ultrasound in clinical settings, it is essential to remain open-minded about the potential it holds. The narrative surrounding ultrasound should shift from a binary perspective of “useful or not” to a more nuanced understanding of how it can complement existing assessment techniques. The ongoing research will need to focus on establishing clear guidelines that configure ultrasound’s best practices in the context of geriatric care.
The challenges inherent in diagnosing sarcopenia underscore a broader issue within healthcare: the often-overlooked complexities of managing chronic conditions in older adults. As experts in the field initiate dialogue about appropriate treatment pathways, the conversation surrounding muscle imaging serves as a microcosm of the larger narrative in age-related health reform. The move towards personalized medicine highlights the need for assessments tailored to individual patient profiles, emphasizing the value of technology in accurately targeting interventions.
The authors’ correction prompts critical reflection on the state of muscle health in older populations and the tools available for clinicians. With the aging demographic steadily increasing globally, adapting our healthcare practices in tune with emerging research must remain a priority. Ultimately, addressing sarcopenia rules out the chance for complacency; instead, it necessitates a proactive approach fueled by innovation in diagnostic technologies.
Conclusively, while muscle ultrasound presents both potential and challenges in assessing sarcopenia, the future remains optimistic. With dedicated research aimed at overcoming current limitations and promoting interdisciplinary collaboration, the aspiration is to reveal how this imaging technique could enhance our approaches to prevention and treatment. The journey to optimal muscle health in older adults hinges on a collective effort fueled by curiosity, precision, and a commitment to improving quality of life. The discussions initiated by the researchers serve not just as an update in the field, but as an invitation for continued exploration and awareness in a segment of health that demands our utmost attention.
Continued research will ultimately determine whether muscle ultrasound can solidify its place in the routine assessment arsenal for sarcopenia, paving the way for breakthroughs that will mitigate the challenges faced by this growing demographic. As patient populations become more diverse and complex, the need for versatile, reliable, and innovative diagnostic tools has never been more apparent. Engaging with the future of muscle health is an endeavor that calls upon the entire healthcare community.
Subject of Research: Sarcopenia and muscle ultrasound technology.
Article Title: Publisher Correction: The sarcopenia conundrum: why muscle ultrasound does (or does not) have a future.
Article References:
Perkisas, S., Welch, C. & Soulis, G. Publisher Correction: The sarcopenia conundrum: why muscle ultrasound does (or does not) have a future.
Eur Geriatr Med (2025). https://doi.org/10.1007/s41999-025-01350-5
Image Credits: AI Generated
DOI:
Keywords: Sarcopenia, muscle ultrasound, aging population, diagnostic tools, muscle health assessment.
Tags: complexities of muscle ultrasoundconsequences of muscle loss in agingearly identification of sarcopeniafrailty and mortality risksfuture of muscle assessment techniqueshealth impairments in older adultsmedical imaging technologies for muscle healthmuscle assessment in older adultsnon-invasive muscle imagingportable ultrasound for bedside assessmentsarcopenia diagnosis and monitoringultrasound technology in geriatric care