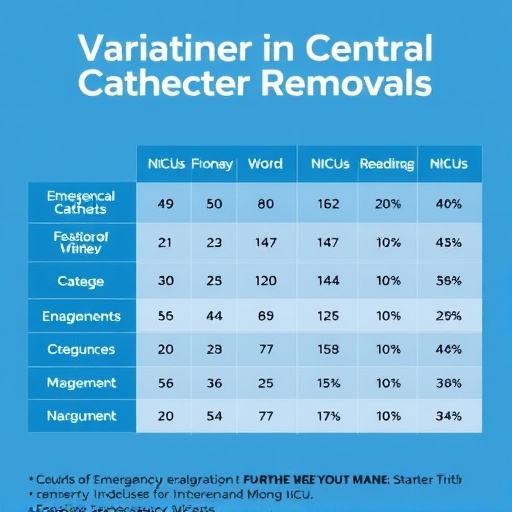
In a groundbreaking study poised to redefine protocols in neonatal intensive care, researchers have meticulously examined the disparities in the rates of non-elective removal (NER) of central venous catheters (CVCs) across level 4 Neonatal Intensive Care Units (NICUs). This comprehensive investigation delves into the underlying causes of variation between centers, aiming to illuminate factors that may influence patient outcomes and drive improvements in neonatal vascular access management. Central catheters, vital for delivering essential treatments to critically ill newborns, are often subject to removal when complications arise. Understanding the inter-center variation (ICV) in such removals is critical for optimizing clinical pathways and ensuring the highest standards of care.
The study responds to the pressing need to quantify and comprehend ICV—a factor long suspected to affect neonatal care quality but sparsely quantified at the granular level of vascular access interventions. Central venous catheters in NICUs facilitate the administration of intravenous medications, fluids, nutrition, and blood sampling, rendering their management pivotal. Non-elective removal typically occurs due to catheter-related complications such as infections, thrombosis, malposition, or mechanical failure, all of which can jeopardize neonatal outcomes. Quantifying the variability in NER across leading NICUs sheds light on potential inconsistencies in clinical practice or systemic factors that merit attention.
Key to this inquiry was the aggregation of data from numerous level 4 NICUs, classified as tertiary or quaternary referral centers managing the most critical neonatal patients. By focusing on these top-tier units, the researchers ensured the inclusion of settings where the utilization and complexity of CVCs are highest. The analytical framework assessed the frequency and underlying etiologies of NER events, examining how these rates fluctuated between institutions. This approach provided insight into procedural heterogeneity, clinical decision-making thresholds, and potentially modifiable risk factors within the specialized NICU environment.
One striking revelation from the study was the pronounced degree of ICV observed among the studied units. Despite ostensibly uniform patient care protocols and adherence to central line maintenance bundles, the NER rates exhibited significant divergence. This variation was not merely statistical noise but suggested systemic differences in managing catheter complications or perhaps discrepancies in diagnostic vigilance and response strategies among centers. Understanding these discrepancies opens avenues for targeted interventions aimed at harmonizing practice and minimizing preventable catheter removals.
In analyzing factors contributing to these variations, the authors explored the role of institutional protocols, staff training levels, and access to specialized vascular teams. Differences in line insertion techniques, catheter type selection, and maintenance practices may subtly yet considerably impact the longevity and complication profile of central lines. The investigation called attention to how nuanced clinical judgments—balancing the risk of prolonged catheter dwell time against the perils of premature removal and reinsertion—manifest across diverse unit cultures and resources.
The implications of such inter-center variability extend beyond immediate procedural outcomes. Non-elective CVC removals impose additional risks on vulnerable neonates, including repeated invasive procedures, increased infection risk, and potential delays in critical therapy delivery. Moreover, escalated removal rates can drive increased healthcare costs and burden hospital resources. Hence, the study underscores the urgency for NICUs to benchmark their outcomes against peer institutions and cultivate quality improvement initiatives geared toward reducing unwarranted NERs.
Methodologically, the research harnessed a robust, multi-institutional dataset, leveraging rigorous statistical modeling to isolate meaningful patterns amid confounding clinical variables. Advanced analytics facilitated adjustment for patient acuity, gestational age, and comorbidities, ensuring that observed ICV was attributable to center-level factors rather than case-mix differences. This methodological rigor enhances the reliability of conclusions and reinforces the study’s call for systemic introspection within NICU practices.
The research also paves the way for future explorations into the mechanistic drivers of catheter-related complications prompting NER. For example, microbiological analyses of infection-related line removals and thrombosis screening protocols could yield actionable insights. Additionally, longitudinal follow-up of neonates experiencing NER events may elucidate long-term sequelae, informing risk-benefit assessments regarding catheter management strategies.
Crucially, the study advocates for the dissemination and adoption of best practices identified in centers exhibiting lower NER rates without compromising care quality. These practices may encompass standardized insertion checklists, enhanced nurse and physician training modules, investment in catheter maintenance technology, and multidisciplinary vascular access teams dedicated to line preservation. Such integrative approaches have the potential to harmonize care across NICU landscapes and mitigate unwarranted procedural burdens on fragile neonates.
An intriguing aspect of the study lies in its capacity to stimulate dialogue on resource allocation and health policy. The observed disparities in NER suggest variability in institutional investment in infrastructure and human capital devoted to vascular access management. Addressing these inequalities is pivotal to leveling the playing field, ensuring that every neonate benefits from cutting-edge, evidence-based catheter care regardless of their treatment center.
Moreover, the findings bear relevance beyond NICU settings, resonating with broader healthcare challenges surrounding device management and removal practices. The concept of inter-center variation is a universal healthcare quality metric, and insights gained from neonatal catheter management may inform analogous efforts in adult critical care, outpatient infusion therapy, and surgical disciplines reliant on indwelling devices.
In conclusion, the meticulous quantification of inter-center variation in non-elective catheter removal among the highest acuity neonatal units offers an invaluable roadmap for clinicians, administrators, and policymakers striving to elevate neonatal care standards. By elucidating the contours of variability, the study catalyzes targeted quality improvement endeavors and lays a foundation for reducing preventable catheter-related morbidity. The advancement heralded by this research portends a future where neonatal vascular access management is both scientifically grounded and uniformly excellent, ultimately improving outcomes for the smallest and most vulnerable patients.
As the neonatal care community digests these insights, the challenge now rests in translating data into action—implementing harmonized protocols, fostering collaborative learning across centers, and investing in innovations that preserve central line integrity. This research epitomizes the power of comprehensive data analysis to uncover hidden variation, spark transformative change, and, most importantly, safeguard the health of newborns entrusted to intensive care.
Subject of Research: Inter-center variation in non-elective removal of central venous catheters in level 4 Neonatal Intensive Care Units.
Article Title: Inter-center variation in non-elective removal of central catheters amongst level 4 NICUs.
Article References:
Beard, L.A., Zaniletti, I., Grover, T.R. et al. Inter-center variation in non-elective removal of central catheters amongst level 4 NICUs. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02478-9
Image Credits: AI Generated
DOI: 13 November 2025
Tags: central catheter removal protocolscentral venous catheter managementcritical care for newbornsinter-center variation in NICUsneonatal catheter-related infectionsneonatal intensive careneonatal vascular access complicationsNICU clinical practice variabilitynon-elective catheter removaloptimizing neonatal care standardspatient outcomes in neonatal carevascular access interventions in neonatology