In a groundbreaking study published in Nature Communications, researchers have unveiled the discovery of a non-canonical lymphoblast subtype that plays a pivotal role in refractory childhood T-cell leukemia. This finding could mark a revolutionary step forward in our understanding of treatment-resistant leukemia, a form of cancer that haunts the prognosis of many young patients worldwide. The study, led by Lim, Whitfield, Trinh, and their colleagues, sheds light on the cellular complexities that underlie the disease’s persistence in the face of conventional therapies.
Childhood T-cell leukemia represents a particularly aggressive subset of acute lymphoblastic leukemia (ALL), characterized by poor outcomes when standard chemotherapy regimens fail. The researchers focused their investigation on refractory cases — instances where the leukemia cells refuse to respond or relapse soon after treatment. By employing advanced single-cell analysis and molecular profiling techniques, the team was able to identify an atypical lymphoblast population that defies canonical definitions.
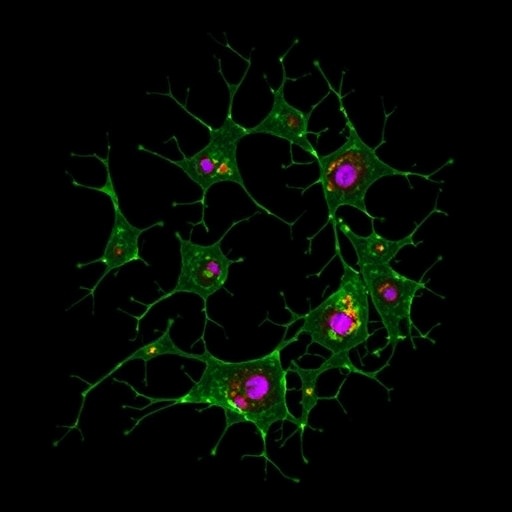
These non-canonical lymphoblasts exhibit a distinct transcriptional and epigenetic signature that diverges significantly from the classical leukemic blasts commonly described in T-cell leukemia literature. Unlike their canonical counterparts, these cells possess unique phenotypic and functional traits, which confer a survival advantage and therapeutic resistance. This nuance was overlooked in previous studies that relied on bulk population analyses, underscoring the importance of high-resolution single-cell approaches.
Delving deeper, the researchers uncovered that these non-canonical lymphoblasts maintain a transcriptional program reminiscent of early thymocyte progenitors but with aberrations that enable unchecked proliferation. This developmental arrest appears to contribute to their resilience, as they evade apoptotic signals typically induced by chemotherapeutic agents. Furthermore, these cells exhibit altered cell surface markers and signaling pathways, including dysregulated Notch1 and MAPK cascades, which have been implicated in leukemogenesis and drug resistance.
The identification of this novel cell population was made possible by integrating single-cell RNA sequencing (scRNA-seq) with chromatin accessibility assays such as ATAC-seq, painting a comprehensive portrait of the epigenomic landscape that sustains their malignancy. The researchers’ bioinformatic analyses revealed distinct enhancer configurations and transcription factor binding profiles, suggesting that these lymphoblasts harness specific regulatory networks to maintain their pathological state.
Crucially, the study highlights how this non-canonical lymphoblast population contributes to the failure of standard chemotherapy regimens. Traditional treatments targeting proliferative canonical blasts may insufficiently address these refractory cells, which can persist as a reservoir responsible for disease relapse. Thus, the findings necessitate a paradigm shift in therapeutic design, emphasizing the need to target these unique cells to achieve durable remission.
The researchers also demonstrated how patient-derived xenograft models recapitulate the presence and behavior of these atypical lymphoblasts, validating their clinical relevance. By using these models, the team was able to test potential therapeutic interventions aimed at disrupting the survival mechanisms of the refractory cells, including inhibitors targeting epigenetic regulators and survival signaling pathways.
This discovery has far-reaching implications for personalized medicine approaches in oncology. It advocates for precision diagnostics that can discern the presence of such non-canonical cells early in the treatment process, guiding clinicians toward combinatorial or alternative therapies better suited to overcoming drug resistance. It also inspires renewed efforts to uncover similar resistant cell populations in other hematological malignancies.
The study’s insights into the molecular underpinnings of refractory T-cell leukemia underscore the complexity of cancer cell heterogeneity and the adaptive tactics employed by malignant cells to escape eradication. They also demonstrate the power of modern single-cell technologies in unraveling these intricate biological processes that have long impeded successful treatment outcomes.
Importantly, the researchers caution against oversimplified therapeutic strategies that fail to account for the dynamic and heterogeneous nature of leukemia. Moving forward, drug development pipelines may need to include compounds that not only kill rapidly dividing blasts but also reprogram or eliminate these resistant lymphoblasts, potentially through epigenetic modulation or interference with key survival pathways.
By unmasking this non-canonical lymphoblast subpopulation, Lim and colleagues have opened a new frontier in our battle against childhood leukemia. Their work exemplifies the marriage of cutting-edge technology and clinical insight, poised to translate into innovative therapies that could one day improve survival rates and quality of life for countless children afflicted by this devastating disease.
Finally, this study exemplifies how precision oncology is evolving, leveraging detailed cellular maps to design smarter, more effective interventions. The immune landscape within leukemic bone marrow is now revealed to be more intricate and nuanced than ever imagined, necessitating a holistic reevaluation of current treatment frameworks.
As researchers around the globe grapple with the clinical challenges of refractory leukemia, the discovery of these non-canonical lymphoblasts provides both a beacon of hope and a call to action. The narrative of T-cell leukemia treatment is being rewritten, with the promise that next-generation therapies will soon outpace the cunning of cancer’s most elusive cells.
Subject of Research: Refractory childhood T-cell leukemia and identification of a non-canonical lymphoblast cell subtype.
Article Title: A non-canonical lymphoblast in refractory childhood T-cell leukaemia.
Article References:
Lim, B.S.J., Whitfield, H.J., Trinh, M.K. et al. A non-canonical lymphoblast in refractory childhood T-cell leukaemia. Nat Commun 16, 9397 (2025). https://doi.org/10.1038/s41467-025-65049-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41467-025-65049-8
Tags: acute lymphoblastic leukemiaadvanced cancer research methodologieschildhood T-cell leukemialeukemia relapse mechanismsmolecular profiling in cancernon-canonical lymphoblast subtypepediatric cancer prognosisrefractory leukemia researchsingle-cell analysis techniquestherapeutic resistance in leukemiatranscriptional epigenetic signaturestreatment-resistant leukemia