In a groundbreaking study poised to reshape neonatal respiratory care, researchers have unveiled critical insights into the relationship between gestational age (GA) and postmenstrual age (PMA) at the time of successful noninvasive respiratory support (NRS) weaning in preterm infants. The study meticulously analyzed various modalities of noninvasive ventilation, such as noninvasive ventilation with neurally adjusted ventilatory assist (NIV-NAVA), nasal continuous positive airway pressure (nCPAP), and high-flow nasal cannula (HFNC), to decipher the nuanced interplay between infants’ maturity and their ability to wean off respiratory support effectively.
Preterm infants often require respiratory assistance to navigate the challenges posed by immature lungs and underdeveloped respiratory drive mechanisms. NRS is a cornerstone intervention due to its noninvasive nature, yet the factors influencing the timing and success of weaning have remained incompletely understood until now. This new research bridges that knowledge gap by providing compelling evidence of how GA at birth directly impacts the PMA at which successful weaning can be expected, with important implications for optimizing respiratory management and improving long-term outcomes.
Central to the study is the concept of PMA, a critical variable defining an infant’s developmental age since conception, combining gestational age with chronological age after birth. Monitoring PMA at the point of successful weaning encapsulates both the biological maturity and the physiological readiness of the infant to sustain independent respiration. By correlating these parameters with GA, the researchers offered a sophisticated model to anticipate respiratory milestones, potentially transforming neonatal intensive care protocols.
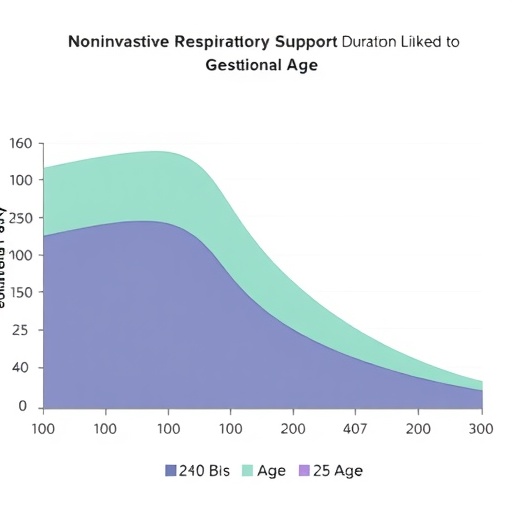
The investigative team employed rigorous statistical analyses across a cohort of preterm infants, stratifying subjects by GA intervals and tracking their progression towards NRS independence. A noteworthy finding is that infants born at earlier GAs generally demonstrated a prolonged requirement for noninvasive respiratory aids, requiring careful stratification to identify those at risk for delayed weaning. This finding underscores the fundamental role of developmental maturity in determining respiratory recovery trajectories.
Equally compelling was the identification of key risk factors extending beyond GA that contribute to delayed NRS weaning. Comorbidities such as bronchopulmonary dysplasia, intraventricular hemorrhage, and persistent pulmonary hypertension emerged as significant modifiers of weaning timelines. These pathological states exacerbate the challenges faced by immature lungs, necessitating enhanced respiratory support duration and complicating clinical decision-making.
One breakthrough aspect of the paper is the elucidation of how varying NRS modalities interact with the infant’s developmental stage. For example, NIV-NAVA, which leverages neural respiratory drive signals to optimize ventilatory assistance, demonstrated bounds of efficacy that are closely tied to the infant’s neural maturation—a factor intrinsically linked to GA and PMA. This mechanistic insight stands to refine personalized respiratory therapies, maximizing weaning success.
Moreover, the research outlines practical implications for neonatal intensive care units (NICUs) globally. The ability to predict the optimal timing of NRS weaning based on GA and other clinical indicators can aid in tailoring respiratory support, minimizing exposure to unnecessary ventilation, and reducing the incidence of ventilation-associated lung injury. This fine-tuning of respiratory management holds promise for enhancing survival rates and neurodevelopmental outcomes in the most vulnerable preterm populations.
The study also sheds light on longitudinal implications, as the duration of NRS impacts not only immediate respiratory outcomes but also longer-term pulmonary function and neurodevelopment. Early and accurate weaning could mitigate risks associated with prolonged respiratory assistance, such as infection and ventilation-induced lung injury, potentially preserving lung architecture and immune competency.
Intriguingly, the research highlights how advances in neonatal ventilatory technology, particularly modalities like NIV-NAVA, call for an integrated understanding of respiratory physiology and developmental biology. By aligning technological capabilities with neonatal developmental benchmarks, clinicians can harness innovative tools in ways that are finely attuned to each infant’s unique maturation timeline.
The data-driven approach employed in this investigation sets new standards for perinatal research methodologies. By blending detailed clinical monitoring with sophisticated statistical modeling, the authors provided robust and clinically actionable evidence, enhancing the predictive power available to neonatal care teams. This represents a step-change from traditional protocols relying on static timelines toward dynamically tailored respiratory care.
Additionally, this study emphasizes the importance of multidisciplinary collaboration, involving neonatologists, respiratory therapists, and neurodevelopmental specialists working in concert to translate research insights into bedside interventions. Such collective effort is pivotal for developing standardized protocols that incorporate GA and PMA as fundamental criteria for respiratory weaning readiness.
As the neonatal field progresses, integrating molecular biomarkers and real-time physiological monitoring with GA and PMA data could further refine individualized respiratory support strategies. This study lays a solid foundation for future research exploring the intersection of genetic predispositions, environmental factors, and developmental physiology in shaping respiratory outcomes.
Ultimately, the findings bear significant implications for clinical practice guidelines, encouraging the adoption of assessment frameworks that prioritize developmental maturity alongside conventional clinical indicators. This paradigm shift promises to optimize respiratory support duration, prioritize infant safety, and accelerate recovery pathways.
In conclusion, the rigorous investigation into the duration and timing of noninvasive respiratory support in preterm infants conducted by Eguchi, Takeda, and Nakao illuminates the critical role of gestational age and other risk factors in shaping respiratory weaning outcomes. By advancing our understanding of the maturation-dependent dynamics of ventilation weaning, this work empowers neonatologists with new tools and insights to elevate care quality and improve prognoses in this vulnerable patient population.
This study marks a pivotal advance in neonatal respiratory medicine, heralding an era where interventions are precisely calibrated to the developmental trajectory of each infant. As research continues to decode the interplay between biological maturation and respiratory physiology, the future holds exciting prospects for increasingly effective, compassionate, and individualized neonatal care.
Subject of Research: Duration of noninvasive respiratory support in preterm infants and its association with gestational age, along with risk factors influencing delayed weaning.
Article Title: Duration of noninvasive respiratory support in preterm infants: Association with gestational age and risk factors for delayed weaning.
Article References:
Eguchi, S., Takeda, T. & Nakao, A. Duration of noninvasive respiratory support in preterm infants: Association with gestational age and risk factors for delayed weaning. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02492-x
Image Credits: AI Generated
DOI: 07 November 2025
Tags: factors affecting respiratory support weaninggestational age and respiratory weaninghigh-flow nasal cannula use in infantsimplications of gestational age on outcomesmodalities of noninvasive ventilationneonatal respiratory management strategiesneurally adjusted ventilatory assist in neonatologynoninvasive respiratory support in preterm infantsoptimizing respiratory care for preterm babiespostmenstrual age in neonatal carepreterm infant respiratory challengesunderstanding postmenstrual age in neonatal health