In the intricate landscape of neonatal brain injuries, groundbreaking research has unveiled a nuanced understanding of how immune cells respond to hypoxic-ischemic insults in the developing brain. Neonatal hypoxic-ischemic encephalopathy (HIE) remains a devastating condition, with survivors often facing lifelong neurological complications. Recent findings published in Nature Communications by Richter et al. shed light on the sequential recruitment and dynamic phenotypes of neutrophils—the frontline immune responders—within the injured neonatal brain. This discovery not only deepens our mechanistic insights into post-injury neuroinflammation but opens doors for targeted immunomodulatory strategies aimed at improving outcomes in affected infants.
Hypoxic-ischemic brain injury occurs when a critical reduction in oxygen and blood flow causes cellular and tissue damage, triggering pathological cascades that include oxidative stress, excitotoxicity, and inflammation. Neutrophils, a subset of innate immune cells typically involved in microbial defense, are now recognized to play dual roles in this scenario. The study by Richter and colleagues meticulously delineates this duality by demonstrating that following neonatal hypoxia-ischemia, neutrophils are not a homogenous population; rather, two distinct subpopulations emerge sequentially, each exerting contrasting effects on the injured brain milieu.
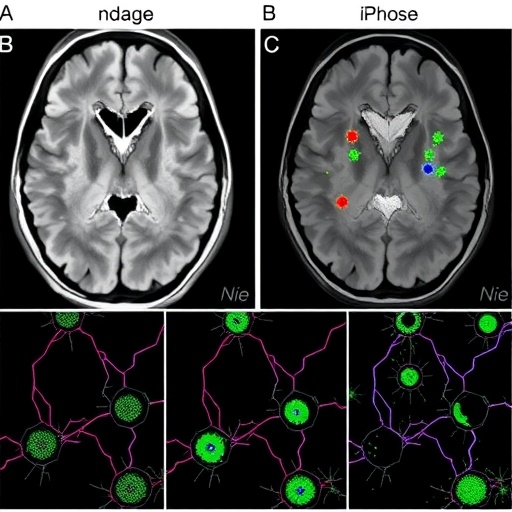
The research utilized a well-established murine model of neonatal hypoxic-ischemic brain injury, allowing the temporal dissection of immune responses within the immature neural environment. Using advanced flow cytometry, transcriptomics, and immunohistochemistry techniques, the team tracked neutrophil dynamics at multiple post-injury time points. Early after injury, neutrophils infiltrating the brain exhibited a predominantly pro-inflammatory phenotype characterized by high expression of reactive oxygen species (ROS) and elevated production of inflammatory cytokines. This initial wave actively contributed to exacerbating neuronal damage and amplifying local inflammation.
Interestingly, a second wave of neutrophils appeared later, marked by anti-inflammatory and reparative characteristics. This population showed enhanced expression of factors involved in tissue remodeling and resolution of inflammation, such as arginase-1 and transforming growth factor-beta (TGF-β). It implies a built-in regulatory mechanism within the innate immune response, where neutrophils adopt a dichotomous phenotype—first amplifying injury, then facilitating repair. This temporal plasticity challenges the traditional view of neutrophils solely as deleterious agents and highlights their multifaceted role in neonatal brain injury.
Further molecular analysis revealed that the microenvironment of the injured brain critically influences this phenotypic switch. Hypoxia-inducible factors (HIFs) and cytokine gradients sculpt the neutrophil functional states, suggesting that targeting these pathways might modulate neutrophil actions therapeutically. For example, modulating HIF signaling could feasibly encourage earlier transition to the reparative phenotype, potentially mitigating long-term neurological deficits by dampening inflammation-driven tissue destruction.
The implications of these findings are profound for clinical translation. Current therapeutic options for neonatal HIE, such as therapeutic hypothermia, offer limited efficacy and do not address the underlying immune dysregulation. By identifying distinct neutrophil populations with divergent functions, Richter et al. propose that selective manipulation of these subtypes could become a viable immunotherapeutic strategy. This could involve suppressing the initial harmful neutrophil infiltration or promoting the later beneficial reparative neutrophils, thereby harnessing the immune system’s inherent capabilities to optimize brain repair.
Moreover, the study underscores the importance of temporal precision in immune interventions. Any therapeutic approach must consider the dynamic shifts in neutrophil phenotypes over the post-injury timeline to avoid counterproductive outcomes. For instance, indiscriminate depletion of neutrophils could hinder repair processes if reparative neutrophils are also eliminated. Hence, precise biomarkers distinguishing neutrophil subsets are essential for developing targeted therapeutics.
This research also adds a new layer to our fundamental understanding of neuroimmune interactions in the neonatal brain. It highlights the complexity of immune cell plasticity and the delicate balance between inflammation and repair necessary for proper recovery after injury. By leveraging such insights, future studies can explore combinatorial treatments pairing immune modulation with neuroprotective agents, aiming for synergistic enhancement of brain resilience and regeneration.
Additionally, these findings could influence investigations into other neuroinflammatory conditions observed in the developing brain, extending beyond hypoxic-ischemic injury. Disorders such as neonatal stroke, infection-induced brain injury, and certain neurodevelopmental disorders may involve similar immune dynamics. The concept of dichotomous neutrophil function might thus be a unifying theme in various pediatric neuropathologies.
From a methodological standpoint, the multi-dimensional approach employed by Richter and colleagues—combining in vivo murine modeling with detailed phenotypic and transcriptional profiling—sets a new standard for studying immune responses in neonatal neuropathology. Their robust dataset enables a granular understanding of cellular mechanisms, paving the way for systems biology analyses integrating immune, neural, and metabolic pathways.
Importantly, the study advocates for future research focusing on how environmental and genetic factors influence neutrophil recruitment and phenotype switching in neonatal brain injury. Understanding inter-individual variability could help tailor personalized therapeutic interventions, improving prognostic accuracy and treatment efficacy. For example, predisposing genetic polymorphisms affecting immune regulation might render some infants more susceptible to detrimental neutrophil responses.
In conclusion, this pivotal study elucidates the dual and sequential roles of neutrophils during neonatal hypoxic-ischemic brain injury, with significant implications for therapeutic innovation. By revealing how the innate immune system transitions from damaging to healing phases via neutrophil phenotypic plasticity, the research offers promising avenues to mitigate neurological impairments in newborns. These insights underscore the evolving paradigm that immune cells are not mere bystanders but active participants shaping neurodevelopmental outcomes after injury.
As neonatal medicine continues to advance, integrating immunology with neuroscience will be key to unlocking novel treatments for complex brain injuries. The work of Richter et al. not only enriches scientific knowledge but also fuels hope for vulnerable infants and their families by moving closer to targeted, effective interventions that harness the body’s own defense mechanisms to promote neural recovery and long-term health.
Subject of Research: Neonatal hypoxic-ischemic brain injury and the role of neutrophil subpopulations in neuroinflammation and repair.
Article Title: Hypoxic-ischemic brain injury in neonatal mice sequentially recruits neutrophils with dichotomous phenotype and function.
Article References:
Richter, M., Diesterbeck, E., Pylaeva, E. et al. Hypoxic-ischemic brain injury in neonatal mice sequentially recruits neutrophils with dichotomous phenotype and function. Nat Commun 16, 9696 (2025). https://doi.org/10.1038/s41467-025-65517-1
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41467-025-65517-1
Tags: dual-phase immune responseexcitotoxicity and inflammationhypoxic-ischemic encephalopathyimmune cell dynamics in neonatesmurine model of HIEneonatal brain injuryneonatal immune responseneonatal neuroinflammationneurological complications in survivorsneutrophil response in brain injuryoxidative stress in brain injurytargeted immunomodulatory strategies