In the intricate landscape of cardiovascular research, a groundbreaking discovery has illuminated new pathways for combating one of the most insidious vascular diseases: abdominal aortic aneurysm (AAA). Luo, Chen, Zhong, and their colleagues have unveiled the pivotal role of Ras-related protein 2 (Rap2) in governing vascular smooth muscle cell (VSMC) behavior—a revelation with profound implications for therapeutic intervention in AAA. This newly published study in Nature Communications reveals that Rap2 acts as a molecular gatekeeper, curbing the phenotypic switching of VSMCs, a cellular transformation now recognized as a central driver in aneurysm pathogenesis.
AAA represents a localized dilation of the abdominal aorta, leading to a weakened vessel wall prone to rupture—a catastrophic event with high mortality rates. Despite advancements in surgical techniques, effective pharmacological treatments remain elusive, largely due to incomplete understanding of underlying molecular mechanisms. Vascular smooth muscle cells, which normally maintain the vessel’s structural integrity, can undergo phenotypic switching from a contractile state to a synthetic phenotype that favors extracellular matrix remodeling, inflammation, and vessel wall weakening. The regulation of this switch is critically important, yet complex and poorly delineated until now.
The study rigorously demonstrates that Rap2 expression inversely correlates with VSMC phenotypic switching. Normally, VSMCs maintain a contractile phenotype characterized by high expression of proteins such as smooth muscle α-actin, essential for vascular tone and stability. However, under pathological stimuli, these cells transition towards a synthetic phenotype, marked by decreased contractile proteins and increased proliferative and migratory capabilities, facilitating aneurysm progression. Luo and colleagues showed that enhanced Rap2 activity stabilizes the contractile phenotype, thereby limiting the cascade of deleterious cellular events leading to aneurysm formation.
At the molecular level, Rap2 operates within the small GTPase family, molecules known for their regulatory roles in cell morphology, proliferation, and gene expression. This study delves into the signaling pathways modulated by Rap2, identifying its interaction with key intracellular effectors that govern cytoskeletal dynamics and gene transcription linked to VSMC identity. By activating pathways that reinforce contractile gene expression and suppressing those promoting phenotypic switching, Rap2 emerges as a master regulator, orchestrating cellular fate decisions critical to vascular homeostasis.
Animal models recapitulating human AAA were employed to validate the protective role of Rap2 in vivo. Transgenic mice with overexpressed Rap2 demonstrated markedly reduced aneurysm incidence and severity compared to control groups. Their aortic tissues exhibited preserved VSMC contractile markers and diminished inflammatory infiltration, underscoring Rap2’s multifaceted protective mechanism. Conversely, models with Rap2 suppression revealed exacerbated aneurysm pathology, confirming the protein’s essential function in maintaining vascular integrity.
Furthermore, the research elucidates the interplay between Rap2 and known inflammatory signals implicated in aneurysm formation. Inflammatory cytokines and oxidative stress are potent inducers of VSMC phenotypic switching. Rap2 appears to counteract these stimuli by modulating downstream effectors such as MAPK and NF-κB pathways, which are notorious for driving inflammatory gene expression. This dual action—both stabilizing VSMC phenotype and dampening inflammation—frames Rap2 as a uniquely appealing target for therapeutic development.
The translational potential of these findings cannot be overstated. Current clinical management of AAA largely depends on monitoring aneurysm size and surgical repair when thresholds are exceeded. There exists a critical need for disease-modifying drugs that can halt or reverse aneurysm progression. Targeting Rap2 or its associated signaling pathways opens an innovative avenue for pharmacological intervention. Small molecules, gene therapy, or biologics designed to enhance Rap2 activity could theoretically restore VSMC contractile phenotype, preserve vascular structure, and reduce rupture risk.
This study also shines a spotlight on the complexity of VSMC phenotypic plasticity, challenging simplistic binary views of contractile versus synthetic states. The researchers propose a nuanced model in which VSMC phenotypes dynamically respond to microenvironmental cues, with Rap2 serving as a genetic and biochemical rheostat fine-tuning these responses. This conceptual advance enhances our understanding of vascular biology and might influence research across a spectrum of vascular diseases involving VSMC dysfunction.
In addition to its implications for AAA, the discovery of Rap2’s role may have broader significance in atherosclerosis, restenosis after angioplasty, and other conditions marked by aberrant VSMC behavior. The conserved nature of Ras-related pathways suggests that this protein’s regulatory functions could extend to other cell types and vascular contexts, representing a common node capable of influencing disease outcomes.
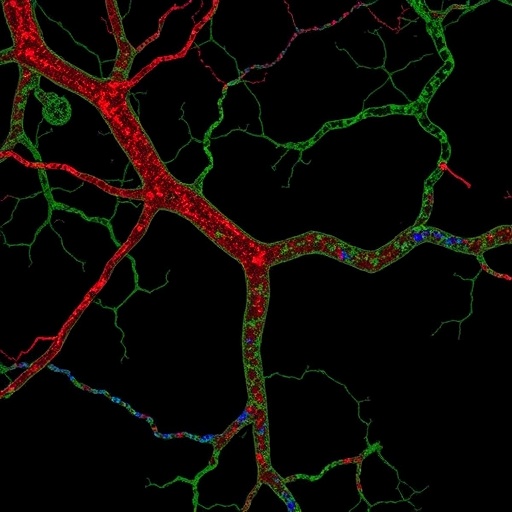
The editorial significance of this paper lies not only in its meticulous molecular characterization but also in its integration of molecular, cellular, and in vivo data to build a compelling narrative. The authors utilized cutting-edge techniques including gene editing, transcriptomic analyses, and advanced imaging to delineate the Rap2-VSMC axis. Their translational approach—from bench to animal models—serves as a paradigm for cardiovascular research aimed at unmasking actionable molecular targets.
As the field presses forward, future research inspired by these findings will likely explore the development of Rap2 agonists and dissect the protein’s interactions with other cellular pathways. Clinical trials designed to evaluate targeted therapies modulating Rap2 activity could emerge as a new frontier in vascular medicine. Moreover, biomarker studies may assess Rap2 expression levels for risk stratification or as indicators of treatment response in AAA patients.
In conclusion, the work by Luo et al. ushers in a transformative perspective on AAA pathophysiology by defining Rap2 as a critical molecular brake on VSMC phenotypic switching and aneurysm progression. Its revelation intertwines fundamental cellular biology with urgent clinical needs, paving the way for innovative therapeutic strategies against a devastating vascular disease. As the scientific community digests this landmark study, the promise of Rap2-targeted interventions kindles optimism for reducing the global burden of abdominal aortic aneurysms.
Subject of Research: Vascular smooth muscle cell phenotypic switching and abdominal aortic aneurysm development
Article Title: Ras-related protein 2 limits vascular smooth muscle cell phenotypic switching and abdominal aortic aneurysm development
Article References:
Luo, S., Chen, J., Zhong, K. et al. Ras-related protein 2 limits vascular smooth muscle cell phenotypic switching and abdominal aortic aneurysm development. Nat Commun 16, 9460 (2025). https://doi.org/10.1038/s41467-025-64496-7
Image Credits: AI Generated
Tags: abdominal aortic aneurysm preventionaneurysm pathogenesis mechanismscardiovascular research breakthroughsextracellular matrix remodeling in aneurysmsmolecular gatekeeper role of Rap2pharmacological treatments for AAAphenotypic switching in VSMCsRas-related protein 2structural integrity of blood vesselstherapeutic interventions for vascular diseasesvascular disease research advancementsvascular smooth muscle cell behavior