In a groundbreaking study published in BMC Pediatrics, researchers have unveiled an innovative method for predicting bowel necrosis in pediatric patients suffering from acute intussusception. This condition, where one segment of the intestine telescopes into another, poses significant health risks, especially in younger populations. The urgency of accurate prediction is paramount; timely intervention can be the difference between a benign outcome and severe complications, including necrosis.
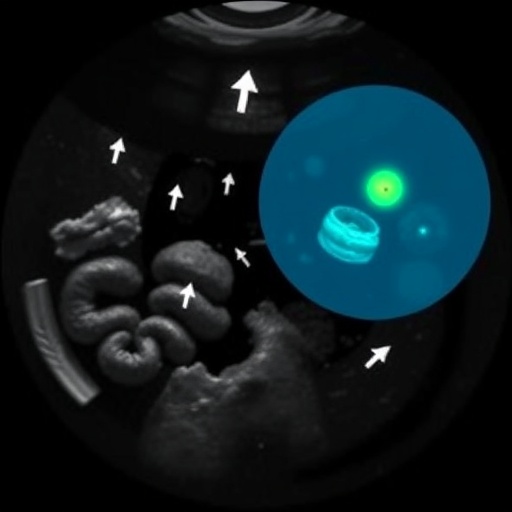
The research, led by Xu and colleagues, delves into a unique integration of anatomical assessments with advanced imaging techniques. Utilizing parameters like intestinal roundness, the study provides clinicians with a valuable predictive tool aimed at enhancing patient outcomes. The implications of these findings could potentially reshape the clinical approach to intussusception in children, marking a significant step forward in pediatric surgical care.
To assess the potential for bowel necrosis, the researchers meticulously analyzed various factors surrounding acute intussusception cases. They established a set of criteria rooted in both clinical observations and quantitative measurements. Among these, the roundness of the affected bowel loops emerged as a critical indicator, allowing healthcare professionals to gauge the likelihood of imminent necrosis. This finding suggests that a more rounded configuration may correlate with lower risks, emphasizing the importance of detailed plasticity assessments in clinical evaluations.
The methodology employed in this research included a comprehensive review of patient records along with advanced imaging studies, primarily ultrasound and CT scans. This two-pronged approach enabled the researchers to gather a robust dataset, ensuring the findings were both extensive and precise. Additionally, the researchers incorporated machine learning algorithms to refine their predictions further, demonstrating a forward-thinking approach to pediatric diagnostics.
With pediatric intussusception presenting in various forms and degrees of severity, the predictive accuracy offered by this study represents a crucial advancement. By identifying children who are at a higher risk for bowel necrosis, surgeons can prioritize timely intervention, thereby mitigating the chances of irreversible damage. This predictive capacity could ultimately lead to a reduction in emergency surgical procedures, alleviating the physical and emotional burden on families.
Furthermore, the attention to roundness as a factor opens new avenues for further research. Future studies could explore the potential link between bowel morphology and other gastrointestinal conditions, potentially leading to broader applications beyond just intussusception. The research team advocates for a paradigm shift in how pediatric cases of gastrointestinal distress are approached, with a greater focus on the anatomical nuances that often go unnoticed.
This pioneering research aligns well with the surge in interest surrounding artificial intelligence and machine learning in healthcare. By combining traditional clinical expertise with modern technological capabilities, the study sets a precedent for future research initiatives aimed at improving diagnostic accuracy through enhanced imaging and algorithmic predictions. It calls for a multidisciplinary approach to pediatric care, encouraging collaboration between surgeons, radiologists, and data scientists.
The findings could also have significant implications for training and education within pediatric surgery. As more medical professionals become attuned to these predictive factors, they can enhance their clinical judgment, transforming the way future generations of surgeons approach acute intussusception. This could lead to a ripple effect, ultimately improving pediatric care on a global scale.
Furthermore, as healthcare systems increasingly turn to evidence-based practices, the ability to predict bowel necrosis using quantifiable measurements fosters a stronger case for implementing these thresholds in clinical guidelines. The urgency for protocol shifts in managing pediatric intussusception will be dependent on the broader adoption of these findings in healthcare policy.
In their conclusion, Xu et al. emphasize the necessity for further validation of their results across diverse populations and healthcare settings. They acknowledge that while their study establishes a foundational understanding of the predictive power of bowel roundness, ongoing research is critical. Through clinical trials and collaborative studies, the ultimate goal remains to fortify the diagnostic toolkit available to pediatric healthcare providers.
As this study garners attention in the medical community, it serves as a potent reminder of the critical intersection between traditional surgical practices and modern technological advances. The integration of new methodologies in analyzing familiar conditions can lead to transformative changes in how we predict and treat pediatric illnesses. It heralds an era in pediatric surgery characterized by a greater emphasis on precision and data-driven decision-making.
Overall, as healthcare professionals digest these findings, there’s potential for a significant paradigm shift in the treatment and management of pediatric intussusception, underscoring the timeless principle of seeking knowledge and advancements in the ever-evolving field of medicine. This research not only enhances the understanding of a common pediatric condition but also paves the way for further innovations in predictive analytics within healthcare.
Subject of Research: Predicting bowel necrosis in pediatric acute intussusception using roundness and other related factors.
Article Title: Predicting bowel necrosis in pediatric acute intussusception using roundness and other related factors.
Article References:
Xu, XX., Cai, YJ., Liu, J. et al. Predicting bowel necrosis in pediatric acute intussusception using roundness and other related factors.
BMC Pediatr 25, 843 (2025). https://doi.org/10.1186/s12887-025-06172-9
Image Credits: AI Generated
DOI: 10.1186/s12887-025-06172-9
Keywords: pediatric intussusception, bowel necrosis, roundness, predictive modeling, machine learning, pediatric surgery.
Tags: acute intussusception imaging techniquesadvanced diagnostic methods for intussusceptionassessing bowel health in pediatric patientsbowel loop analysis in intussusceptionclinical predictors of bowel healthemergency interventions for bowel necrosisenhancing outcomes in pediatric surgeriesinnovative approaches to pediatric careintestinal roundness in childrenpediatric intussusception assessmentpediatric surgical interventionspredicting bowel necrosis