A groundbreaking study from the University of Cambridge’s Loke Centre for Trophoblast Research has shed new light on the intricacies of early human embryo development, challenging current paradigms in fertility medicine. For years, fertility clinics worldwide have relied on pre-implantation genetic testing for aneuploidy (PGT-A) to screen embryos created via IVF for chromosomal abnormalities. However, this novel research reveals that such tests, conducted on biopsies taken from the outer layer of blastocysts, may overestimate abnormalities that do not necessarily compromise fetal health.
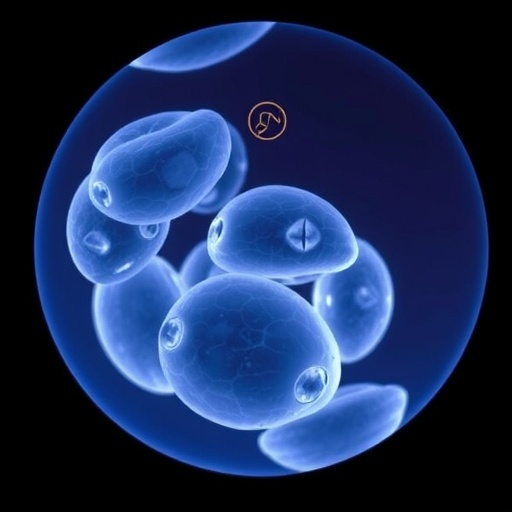
At the heart of human reproduction, the journey from a single fertilized egg—or zygote—to a complex organism begins with multiple rounds of cell division. During this process, the embryo evolves into a blastocyst, a hollow sphere composed of an outer layer destined to form the placenta and an inner cell mass that gives rise to the fetus. Traditionally, genetic testing targets cells from this outer layer just prior to implantation into the uterine wall, aiming to assess chromosomal normality and embryo viability. Yet, the new findings suggest that chromosomal abnormalities detected in these outer cells may arise later in development, predominantly affecting the placenta rather than the embryo proper.
The team’s pioneering approach involves real-time live imaging of human embryos, employing advanced light-sheet fluorescence microscopy. By tagging DNA within the nuclei with fluorescent proteins, researchers were able to observe the embryos in three dimensions over extended periods without inflicting damage. This represents a significant technical leap, as previous imaging attempts either lacked the necessary resolution or compromised the integrity of the sensitive embryos.
Lead scientist, Professor Kathy Niakan, emphasizes the clinical implications: “Our research demonstrates that errors in chromosome segregation can occur at comparatively late stages, specifically within the trophoblast—the precursor to the placenta—rather than within the inner cell mass that leads to the fetus. This challenges the assumption that all detected aneuploidies are detrimental to embryo viability.” Such a revelation calls into question current IVF protocols that may discard embryos unnecessarily based on biopsy results from placental precursor cells that harbor transient or non-lethal chromosomal anomalies.
During their meticulous investigations, researchers monitored thirteen embryos donated by families with successful pregnancy histories. They discovered that approximately 10% of the observed cells presented chromosomal irregularities, with abnormalities such as chromosome missegregation during mitosis or atypical cell divisions producing three daughter cells instead of the usual two. Crucially, these aberrations manifested predominantly in the trophoblast lineage, highlighting a spatial and temporal separation between embryonic and placental cell development regarding genetic stability.
The imaging modality utilized in this study—light-sheet microscopy—allowed for simultaneous observation of multiple embryos from multiple angles, capturing rare and previously invisible mitotic events. Dr. Ahmed Abdelbaki, first author on the paper, describes how “this gentle yet high-resolution technique permitted continuous monitoring over a two-day interval, unveiling dynamic processes that were hitherto obscured.” These technological advancements unlock unprecedented windows into human embryogenesis, crucial for unraveling the origins of developmental disorders.
Moreover, this research underscores the inherent biological complexity and resilience of early human development. While chromosomal errors in trophoblast cells may not doom the embryo, their presence does bear relevance to placental function and potentially pregnancy outcomes. The placenta’s temporary and supportive nature allows some leeway for genetic variation that may not translate into fetal abnormalities, a nuance that current genetic assays fail to distinguish.
Looking ahead, Professor Niakan’s group plans to extend their investigations into the inner cell mass to determine whether de novo mitotic errors also arise within cells destined to form the fetus. This line of inquiry could refine the predictive value and accuracy of embryo screening methods, minimizing discards of potentially viable embryos and rendering assisted reproductive technology (ART) more efficient and less burdensome for patients.
Infertility remains a profound emotional and financial challenge, with assisted conception witnessing steadily rising demand. However, many embryos generated via IVF fail to survive to the implantation stage. Improvements in understanding the timings and locations of chromosomal abnormalities via cutting-edge live imaging will be crucial to optimizing selection criteria and therapeutic interventions.
The study was made possible by collaborations with the Francis Crick Institute and was funded by leading bodies including the Wellcome Trust and the Medical Research Council. It was recently published in the prestigious journal Nature Biotechnology, signifying a milestone in reproductive biology and translational medicine.
Ultimately, this research calls for a critical reassessment of current PGT-A practices, advocating for techniques that discern between placental and embryonic genetic abnormalities. Such precision could revolutionize embryo selection, improve IVF success rates, and significantly reduce unnecessary treatments and patient distress.
In summary, this study not only pioneers advanced imaging methodologies that deepen our grasp of human embryo development but also provokes vital questions about the interpretation of genetic tests in reproductive medicine. It highlights the remarkable adaptability of early embryos and the importance of aligning diagnostic tools with biological realities.
Subject of Research:
Cells
Article Title:
Live imaging of late-stage preimplantation human embryos reveals de novo mitotic errors
News Publication Date:
23-Oct-2025
Web References:
http://dx.doi.org/10.1038/s41587-025-02851-1
References:
Abdelbaki, A et al. Live imaging of late-stage preimplantation human embryos reveals de novo mitotic errors. Nat Biotech; 23 Oct 2025; DOI: 10.1038/s41587-025-02851-1
Keywords:
Embryology, Developmental biology, Ontogeny
Tags: advancements in fertility researchchallenges in IVF practiceschromosomal abnormalities in IVF embryosearly human embryo developmentimpact of embryo biopsies on fetal healthimplications of genetic testing in fertility medicineIVF embryo assessment techniquesplacenta formation in embryospre-implantation genetic testing for aneuploidyreal-time live imaging of embryosreliability of IVF embryo screeningsignificance of blastocyst development