In a breakthrough study that could redefine our understanding of Parkinson’s disease and its most debilitating motor symptom, researchers have unveiled intricate neural mechanisms underlying turn-induced freezing of gait (FOG). Freezing of gait, a phenomenon where patients experience sudden, transient inability to step forward, especially during turning movements, significantly impairs quality of life and raises the risk of falls among those afflicted with Parkinson’s disease. The newly published findings, emerging from a collaboration between neuroscientists and clinicians, provide unprecedented insights into the phase-specific interactions between cortical and subthalamic brain regions, painting a complex picture of the neural dynamics that precede and sustain freezing episodes.
The investigation zeroes in on the cortico-subthalamic circuitry, a network long implicated in motor control and dysfunction in Parkinson’s. By employing state-of-the-art electrophysiological recording techniques alongside sophisticated computational analyses, the researchers decoded neural oscillations in real-time as patients navigated a turning task designed to reliably provoke FOG. What sets this study apart is its granularity—scrutinizing neural activity at distinct phases within the turning movement, the team mapped how deviations in brain rhythms correspond with the onset and persistence of freezing.
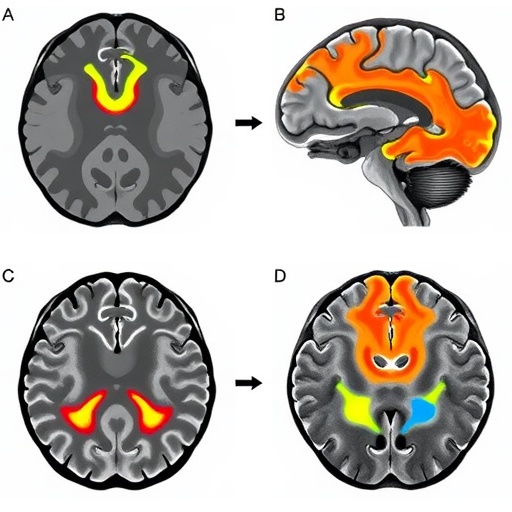
At the heart of these discoveries is the identification of distinct neural signatures in the beta frequency band, a spectral range traditionally linked to motor rigidity and bradykinesia in Parkinson’s disease. During the approach to a turn, heightened beta synchrony between the cortex and subthalamic nucleus appears to herald the imminent freezing episode. This hypersynchronization likely represents an aberrant neural state where motor commands become ‘locked’, preventing fluid movement initiation. The study’s data convincingly argue that turn-induced FOG is not merely a failure in motor execution but rather a dysregulation of the underlying neural circuitry’s timing and coordination.
Further dissecting the cortico-subthalamic dialogue, the team found that pathological beta coupling dominates specifically during the transition phase of the turn, a critical window where gait adjustments normally occur seamlessly. Intriguingly, this maladaptive synchronization declines once the freezing episode ends, suggesting a dynamic, reversible neural signature intimately tied to the motor blockade. This temporal specificity is crucial, as it suggests potential therapeutic windows for interventions aiming to disrupt or modulate beta oscillations precisely when needed to restore locomotion.
Complementing beta-band dynamics, the researchers observed alterations in lower frequency theta oscillations, which may represent compensatory or modulatory efforts by the brain to overcome freezing. This interplay between theta and beta rhythms within the cortico-subthalamic loop unveils a nuanced oscillatory landscape that could be leveraged for developing neuromodulation strategies tailored to the phase-specific neural disturbances that cause FOG.
These findings also hold profound implications for deep brain stimulation (DBS), a mainstay treatment for alleviating motor symptoms in Parkinson’s disease. Traditionally, DBS targeting the subthalamic nucleus operates on a continuous stimulation paradigm, but this study underscores the potential advantage of adaptive DBS systems that respond to specific neural states. By detecting the distinctive beta signatures poised to induce freezing, next-generation DBS devices could deliver targeted pulses to disrupt pathological synchronization at critical movement phases, thereby preventing or aborting freezing episodes more effectively.
The experimental paradigm was meticulously crafted to mirror real-world challenges faced by patients. By analyzing neural data during active turning rather than static or simple walking tasks, the study captures the essence of motor conflicts and cognitive demands that provoke freezing in everyday life. Such ecological validity enriches the translational value of the research, bridging the gap between laboratory findings and clinical realities.
From a methodological perspective, the integration of invasive subthalamic recordings with non-invasive cortical measures presents a holistic view of the motor network’s behavior. This dual vantage point, combined with sophisticated phase-specific analytic frameworks, sets a new standard for studying motor phenomena in movement disorders. The approach holds promise for unraveling other enigmatic motor symptoms beyond freezing, such as dyskinesias or dystonias.
Crucially, the study navigates the complex heterogeneity of Parkinson’s disease, acknowledging that freezing is a multifactorial and variable phenomenon influenced by disease stage, medication status, and individual neural architecture. The identification of a consistent neural fingerprint across patients offers hope for developing universal biomarkers, yet also highlights the necessity for personalized approaches that account for individual neural dynamics when designing interventions.
The implications for patient care are profound. By deepening our understanding of the neural underpinnings of freezing of gait, clinicians may better predict who is at risk and tailor therapeutic plans accordingly. Moreover, the insights open avenues for non-invasive brain stimulation techniques—such as transcranial magnetic stimulation or transcranial alternating current stimulation—targeted at modulating pathological beta activity during vulnerable movement phases, offering less invasive alternatives to surgery.
Beyond therapeutic potentials, these neural signatures could contribute to refined diagnostic tools. Future wearable neurophysiological sensors capable of detecting beta oscillation patterns in everyday settings might alert patients or caregivers to impending freezing events, enabling preemptive behavioral strategies or assistive interventions to mitigate fall risks.
The research team emphasizes that while these findings mark a significant advance, the road ahead involves further validation, especially in larger, more diverse patient populations. Longitudinal studies tracking changes in cortico-subthalamic dynamics over disease progression could elucidate how freezing mechanisms evolve and respond to treatments. The adaptability and plasticity of these circuits also warrant exploration, potentially revealing whether targeted therapies might induce durable neural reorganization.
The study also opens fascinating questions about the broader role of neural oscillations in motor control beyond Parkinson’s disease. Understanding how pathological rhythms disrupt movement initiation and execution may shed light on fundamental neurobiological principles governing motor systems, possibly informing research on stroke, dystonia, or other movement disorders.
In sum, the unveiling of phase-specific cortico-subthalamic dynamics as neural harbingers and mediators of turn-induced freezing of gait crystallizes a critical intersection of neurophysiology, clinical neurology, and biomedical engineering. This paradigm-shifting knowledge not only enriches the scientific narrative on Parkinson’s motor symptoms but also propels the quest for innovative, precision-targeted interventions poised to reclaim mobility and independence for millions worldwide.
As technology advances and multidisciplinary collaborations flourish, the prospect of translating these neural insights into tangible clinical breakthroughs appears more tangible than ever. The dynamic, oscillatory brain—a once elusive frontier—is now yielding its secrets, bringing hope to patients and fueling a new era of neuromodulation therapies that harmonize neural rhythms to restore the grace of movement.
Subject of Research: Neural mechanisms underlying turn-induced freezing of gait in Parkinson’s disease.
Article Title: Neural signatures of turn-induced freezing of gait in Parkinson’s disease: insights from phase-specific cortico-subthalamic dynamics.
Article References:
Zhang, Q., Xie, H., Zhao, B. et al. Neural signatures of turn-induced freezing of gait in Parkinson’s disease: insights from phase-specific cortico-subthalamic dynamics. npj Parkinsons Dis. 11, 305 (2025). https://doi.org/10.1038/s41531-025-01173-y
Image Credits: AI Generated
Tags: Beta frequency band signaturesComputational analyses in neuroscienceCortico-subthalamic circuitryElectrophysiological recording techniquesfreezing of gait in Parkinson’sMotor control and dysfunctionNeural mechanisms of Parkinson’s diseaseNeural oscillations in movementPhase-specific neural dynamicsQuality of life and Parkinson’sRisk of falls in Parkinson’s patientsTurning movements and FOG