In the relentless battle against cancer, metabolic rewiring has emerged as a fundamental hallmark that fuels tumor progression and metastasis. Recent groundbreaking research published in Nature Metabolism unveils a novel metabolic crosstalk within the tumor microenvironment that may redefine therapeutic strategies against hepatocellular carcinoma (HCC), one of the deadliest forms of liver cancer. The study illuminates how tumor-associated macrophages (TAMs), specialized immune cells co-opted by cancer, metabolically contribute to tumor aggressiveness by acting as an acetate reservoir, fundamentally sustaining cancer cell metabolism and metastatic capacity.
Understanding the metabolic vulnerabilities of cancer cells has long been a cornerstone of cancer biology. A critical metabolite in this landscape is acetyl-coenzyme A (acetyl-CoA), a pivotal molecule involved in energy metabolism, lipid synthesis, and epigenetic modulation. Elevated levels of acetyl-CoA have been documented to drive cancer metastasis, yet the precise source of this metabolite within the tumor microenvironment remained elusive. The innovative work spearheaded by Shen and colleagues uncovers that TAMs secrete acetate, a key precursor metabolite, which tumor cells avidly take up to maintain high intracellular acetyl-CoA levels critical for metastatic behavior.
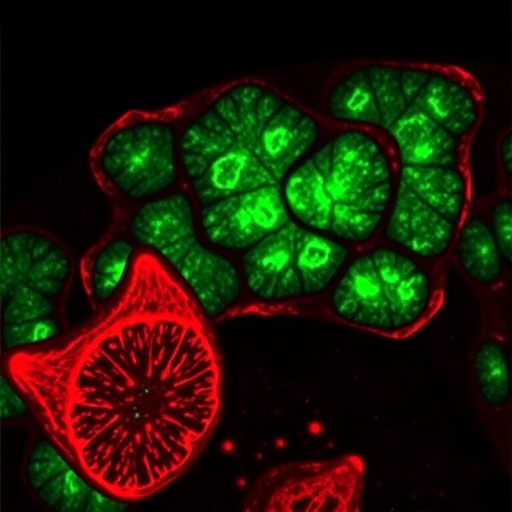
This discovery uncovers a previously unappreciated metabolic symbiosis: HCC tumor cells secrete lactate into their surrounding environment, which paradoxically activates a metabolic pathway in TAMs characterized by lipid peroxidation and the enzymatic activity of aldehyde dehydrogenase 2 (ALDH2). This activation triggers TAMs to convert lipid peroxidation products into acetate, which they then release back into the microenvironment. In essence, HCC cells manipulate TAMs to produce a vital fuel—acetate—creating a reciprocal loop that supports tumor aggressiveness.
Delving deeper into the molecular mechanisms, the study highlights ALDH2 as a linchpin enzyme driving the acetate-producing capability of TAMs. Lipid peroxidation generates reactive aldehydes that can be detoxified and metabolized into acetate by ALDH2. By pharmacologically inhibiting ALDH2 or blocking lipid peroxidation processes within TAMs, the researchers effectively curtailed acetate production. Remarkably, this intervention suppressed the migratory and invasive capabilities of HCC cells in vitro, underscoring the potential therapeutic value of targeting this metabolic axis to restrain cancer dissemination.
The researchers then translated these in vitro findings into an orthotopic HCC mouse model, employing genetic ablation to selectively eliminate ALDH2 within TAMs. This genetic intervention yielded profound reductions in acetate availability within tumor cells and correspondingly led to a marked decrease in lung metastases. These in vivo results validate the pivotal role of TAM-derived acetate in facilitating metastatic spread and potentiate ALDH2 inhibition as a promising anti-metastatic strategy.
This study elegantly bridges the gap between metabolic biochemistry and tumor immunology by portraying TAMs not merely as passive bystanders or immune effectors but as active metabolic accomplices that nurture cancer progression. The metabolic plasticity of TAMs, particularly their ability to harness lipid peroxidation pathways to generate acetate, reveals a layer of complexity in tumor-stroma interactions that had previously gone unappreciated.
The implications of these findings extend beyond HCC, potentially informing understanding in other malignancies where macrophage infiltration and acetate metabolism intersect. Tumors are known to exploit local microenvironmental factors, including immune cells and metabolic substrates, to thrive and metastasize. Un covering the metabolic dialogue that enables such exploitation offers innovative angles for therapeutic intervention, particularly in combating metastasis, the primary cause of cancer mortality.
It is also significant that the study positions lactate, a common metabolic byproduct of cancer cells’ glycolytic metabolism, as a key mediator orchestrating acetate production in TAMs. This recasts lactate from a mere waste product to a signaling molecule within the tumor milieu, modulating immune cell metabolism to favor cancer progression. Such insights contribute to a growing appreciation of lactate’s dual role as a metabolic substrate and an immunomodulatory signal in cancer.
Targeting ALDH2 enzymatic activity emerges as a compelling therapeutic route. Given ALDH2’s role in detoxifying lipid peroxidation aldehydes and facilitating acetate production, inhibiting this enzyme may cripple the metabolic support TAMs provide to tumor cells. This therapeutic approach could synergize with existing treatments, potentially mitigating metastatic dissemination and improving patient outcomes.
Moreover, these findings prompt a re-evaluation of how tumor microenvironments are conceptualized—highlighting the dynamic metabolic interdependencies between cancer cells and surrounding stromal and immune elements. Recognizing that immune cells such as TAMs can serve as reservoirs and factories for critical metabolites may revolutionize strategies to disrupt tumor metabolism at multiple fronts.
The complexity of lipid peroxidation pathways in TAMs, implicated in this acetate production, also invites further investigation. Understanding the specific lipid substrates undergoing peroxidation, and the signals triggering this process in TAMs when exposed to tumor-derived lactate, could reveal additional molecular targets to disrupt this metabolic crosstalk.
In light of these insights, future research may explore how modulation of microenvironmental acetate levels impacts epigenetic modifications in cancer cells, given acetyl-CoA’s pivotal role as a substrate for histone acetylation. This could open avenues linking metabolic regulation by TAMs to the epigenetic reprogramming that underlies metastatic competence.
Equally, the study underscores the need to consider cellular heterogeneity within the tumor microenvironment. TAM subpopulations with varying metabolic profiles might differentially contribute to acetate production and tumor support, suggesting tailored interventions might be required for maximal therapeutic efficacy.
In conclusion, the discovery that tumor-associated macrophages act as an acetate reservoir to drive hepatocellular carcinoma metastasis unveils a sophisticated metabolic alliance that enables aggressive cancer behavior. By dissecting the lactate-induced activation of lipid peroxidation and ALDH2 pathways in TAMs, this research provides a mechanistic understanding that not only advances fundamental cancer biology but also signals new frontiers for therapeutic innovation targeting the metabolic ecosystems supporting metastasis.
Subject of Research: Tumor-associated macrophages as metabolic contributors to hepatocellular carcinoma metastasis through acetate production.
Article Title: Tumour-associated macrophages serve as an acetate reservoir to drive hepatocellular carcinoma metastasis.
Article References:
Shen, L., Wang, S., Gao, C. et al. Tumour-associated macrophages serve as an acetate reservoir to drive hepatocellular carcinoma metastasis. Nat Metab (2025). https://doi.org/10.1038/s42255-025-01393-9
Image Credits: AI Generated
Tags: acetate reservoir in canceracetyl-CoA and cancer metastasishepatocellular carcinoma researchimmune cells and tumor progressionlactate secretion by tumor cellsmacrophages and cancer aggressivenessmetabolic crosstalk in tumorsmetabolic symbiosis in tumorsmetabolic vulnerabilities in cancer cellstherapeutic strategies for liver cancertumor macrophages in liver cancertumor microenvironment and metabolism