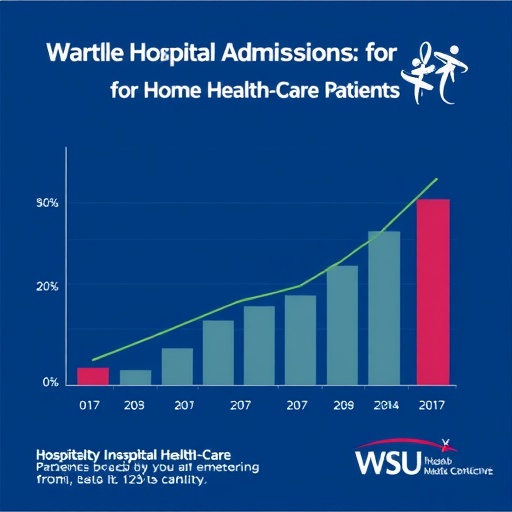
In the realm of home health care, a staggering challenge has persisted largely unnoticed: the pervasive presence of medication discrepancies among patients. Recent findings indicate that approximately 90% of individuals receiving home-based health services carry at least one inconsistency in their medication regimens, a condition that significantly heightens their risk of hospital admission. This widespread issue has prompted a pioneering initiative at Washington State University (WSU), aimed at radically transforming medication management practices in home health care settings through pharmacist-led quality improvement.
The WSU endeavor took root in Spokane, Washington, focusing on a nonprofit home health care agency that manages around 3,500 patient admissions annually. The project’s central mission was to train nurses and other in-home clinicians to “think like pharmacists” when conducting medication reconciliation—a complex process that involves ensuring patient medication lists are accurate, comprehensive, and aligned with actual consumption patterns. This revolutionary approach sought to embed pharmaceutical expertise within the nursing workforce, effectively bridging a gap in the home health care model that traditionally lacks direct pharmacist involvement.
Medication discrepancies often arise due to fragmented communication channels among multiple healthcare providers, including general practitioners, specialists, hospitals, and rehabilitation centers. Each node in this chain typically maintains its own medication records, which may not be synchronized upon patient discharge or transfer. Moreover, medication adherence becomes an additional variable, with patients sometimes deviating from prescribed regimens due to confusion or other factors. This fragmentation and variability culminate in “unreconciled” medication lists, presenting an enduring challenge that significantly elevates patient vulnerability to adverse outcomes, especially hospitalizations.
WSU’s approach incorporated meticulous interdisciplinary teamwork, comprehensive training modules, and the introduction of an innovative reconciliation tool. This tool encompassed a detailed checklist addressing thirteen distinct scenarios wherein medication lists could be misaligned, enabling clinicians not only to match medication data across records but to critically assess the appropriateness, effectiveness, safety, and adherence of each medication as a pharmacist would. This dual focus on accuracy and clinical evaluation represents a paradigm shift, advancing beyond traditional reconciliation practices that merely seek to harmonize electronic records.
The project formally began in late 2018 with the collaboration of pharmacists, nurses, physical therapists, and occupational therapists. A pharmacist-led team developed new protocols to integrate medication evaluation into everyday home health care practice. This initiative empowered clinicians to conduct thorough reviews of patient medication regimens during home visits—taking advantage of their unique positional access to patients’ actual medication use in real time. The comprehensive training emphasized that successful medication optimization demands not only precise record-keeping but also an expert clinical lens to identify potential medication-related issues.
Clinical outcomes from the initiative have been profoundly impactful. In a focused 10-week evaluation period following the implementation of training and tools, hospitalization rates among high-risk heart failure patients dropped precipitously from 23.4% to 11.4%. This achievement is especially notable among patients grappling with two or more unreconciled medications, a subgroup previously documented to have a threefold increased risk of hospital admission within 30 days. The intervention thus demonstrated not only immediate efficacy but also potential for sustainable improvement, as evidenced by a reduction in rehospitalizations over a longer 17-month observation window.
The implications of these results extend beyond the immediate metrics. Jeffrey Clark, associate professor in the College of Pharmacy and Pharmaceutical Sciences at WSU and the study’s corresponding author, emphasized the unique service opportunity presented by home health care. Unlike hospital environments—where clinical pharmacists are routinely embedded—the home health sector commonly operates without such pharmaceutical expertise integrated into patient care teams. Empowering home health clinicians to adopt pharmacist perspectives could therefore reshape medication management paradigms, fostering preventive care and reducing avoidable healthcare utilization.
Underlying the success of this quality improvement project was a shift in the clinical culture surrounding medication management. Traditionally, medication reconciliation efforts have been perceived as administrative or clerical tasks, primarily aimed at updating electronic health records without thorough clinical scrutiny. By embedding pharmacological evaluation into the reconciliation process and training clinicians to apply critical judgment, the project redefined reconciliation as an active, clinically driven process essential to patient safety. This holistic approach highlights the necessity of multidisciplinary collaboration in addressing the complexities of medication management in home health contexts.
Moreover, the methodology deployed by WSU—combining a structured checklist with personal clinical assessment—provides a scalable model for broader implementation. This framework can serve as a template for other home health agencies seeking to diminish medication discrepancies and mitigate associated risks. Crucially, the initiative underscores the value of embedding pharmacists or pharmacist-led training within care teams, potentially influencing healthcare policy and resource allocation toward enhanced medication safety strategies.
This project, supported by a grant from Pfizer, aligns with national efforts to optimize medication use through the Institute of Healthcare Improvement’s Learning Action Network. It stands as a testament to the transformative power of targeted quality initiatives when informed by evidence-based practices and interprofessional collaboration. As healthcare systems worldwide grapple with the challenges of aging populations and complex chronic conditions, such pharmacist-led innovations symbolize a crucial step toward safer, more effective home-based care.
Ultimately, the findings illuminate the pressing need to reassess home health care protocols, recognizing medication reconciliation and evaluation not just as bureaucratic necessities but as vital clinical interventions. The integration of pharmaceutical expertise within home health teams could serve as a linchpin in reducing hospital readmissions, improving patient outcomes, and enhancing overall healthcare sustainability. As the healthcare landscape evolves, embedding pharmacists in home health care promises to be an essential strategy to optimize medication safety and patient well-being.
Subject of Research:
People
Article Title:
A Pharmacist-Led Quality Improvement Project to Optimize Medication Evaluation and Reconciliation in Home Healthcare
News Publication Date:
1-Sep-2025
Web References:
http://dx.doi.org/10.1097/NHH.0000000000001377
References:
Published in the journal Home Health Care Now, DOI: 10.1097/NHH.0000000000001377
Keywords:
Medication reconciliation, home health care, pharmacist-led intervention, medication discrepancies, hospitalization reduction, medication adherence, quality improvement, interdisciplinary teamwork, chronic illness management, heart failure, patient safety, clinical pharmacy
Tags: enhancing medication accuracy in home healthhome health care patient safetyhospital admissions reduction strategiesimproving communication in healthcareinterdisciplinary collaboration in healthcaremedication discrepancies in home caremedication management in home health carenonprofit healthcare agency initiativesnursing training for medication reconciliationpharmacist-led quality improvementSpokane Washington health initiativesWSU home health care initiative