Recent advancements in medical imaging have opened new avenues for the assessment of osteoporosis, particularly in challenging patient populations such as those suffering from ankylosing spondylitis (AS). A pivotal study has emerged, indicating that the use of Hounsfield units (HU) derived from computed tomography (CT) scans may enhance the identification of osteoporosis over traditional dual-energy X-ray absorptiometry (DXA) techniques. This groundbreaking work, which focuses on patients exhibiting a radiological feature referred to as “bamboo spine,” presents a compelling argument for a paradigm shift in how we evaluate bone density and, consequently, osteoporosis risk.
Osteoporosis, characterized by weakened bones and increased fracture risk, remains a significant public health issue affecting millions worldwide. Conventional methods for diagnosing this condition have leaned heavily on DXA scans, which measure bone mineral density (BMD). However, these scans have significant limitations, particularly for patients with alterations in spinal morphology due to conditions like AS. In cases where metaplastic changes occur, the accuracy of BMD assessments can be dramatically compromised, underscoring the need for alternative evaluation techniques.
The study in question employed a CT-based approach utilizing a HU cut-off value of less than 135 to classify patients more effectively. The results revealed that a staggering additional 78% of patients were classified as having osteoporosis when compared to the classifications provided by DXA scans. This discrepancy highlights the insufficiency of DXA evaluations for those with complex spinal conditions, where the conventional assessments fail to capture the nuances of bone density variations.
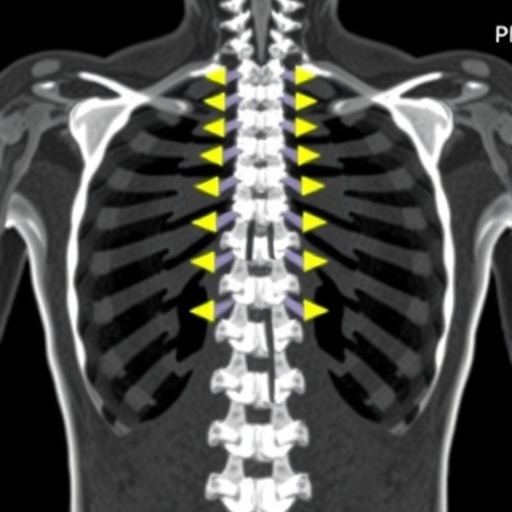
The bamboo spine phenomenon — characterized by the calcification and fusion of spinal segments in AS patients — can often obscure traditional evaluation methods, leading to a potential underestimation of osteoporosis risk. By employing a CT-based analysis and focusing on Hounsfield units, the researchers observed a marked improvement in diagnostic accuracy. It appears that this imaging technique allows for a more nuanced view of the bone architecture, which is essential in the correct classification of osteoporosis in patients with distinctive spinal deformities.
One of the most significant concerns for practitioners is ensuring that diagnostic tools are both accurate and reliable. The utilization of CT imaging has often been more resource-intensive and less accessible than DXA. However, the findings from this study could encourage the adoption of CT scanning as a viable alternative, especially in specialized clinics where high-quality imaging is available. The potential ramifications for patient management are considerable; accurate assessment of osteoporosis risk could lead to timely interventions and improved outcomes for patients in this vulnerable demographic.
Furthermore, the researchers pointed out that relying solely on the DXA-based classification systems could leave many patients without appropriate interventions. The study proposes that the integration of HU metrics derived from CT scans into routine practice may ultimately provide a more comprehensive assessment of skeletal health, particularly in a population predisposed to atypical bone density patterns.
As the medical community continues to evaluate diagnostic modalities, this study emphasizes the need for prospective validation. Larger cohorts and diverse datasets will be essential in confirming the robustness of these findings. Validation studies are crucial, as the implications of misclassification of osteoporosis can lead to either unnecessary treatments or overlooked interventions that could prevent serious complications such as fractures.
This emerging research opens the door for future investigations to explore how CT-based Hounsfield units can be further refined as a metric for assessing osteoporosis. Attention to other factors, including age, sex, and underlying conditions, will be imperative for developing nuanced protocols tailored to different patient populations.
The potential for cross-institutional collaboration to advance this area of research is also promising. By pooling resources and expertise, researchers could enhance the breadth of studies examining the utility of CT in osteoporosis assessments. Such collaborations may facilitate comprehensive training programs for both radiologists and clinicians, ensuring that knowledge about these evolving methodologies is disseminated effectively.
In conclusion, the integration of CT-based Hounsfield units into the osteoporosis assessment framework for ankylosing spondylitis patients represents a significant stride forward in clinical practice. As this research garners attention, it will be essential for practitioners to remain informed and adaptable to these emerging methodologies, which promise to refine the management of bone health in complex populations. By prioritizing accurate diagnoses, the medical community can ultimately enhance the quality of care provided to individuals at risk of osteoporosis.
The dialogue around such research fosters a deeper understanding of the interplay between imaging techniques and patient outcomes. As more studies illuminate the potential benefits of CT over DXA in assessing osteoporosis, healthcare providers must take heed and adapt their practices accordingly. This kind of proactive engagement with emerging data will not only improve disease management but also empower patients with the knowledge and care they deserve.
With these advancements in mind, the focus on patient-centric approaches remains paramount. As we continue to navigate the complexities of osteoporosis diagnosis and treatment, it is crucial to embrace innovative methods and validate them thoroughly within clinical settings. This ensures that all patients, particularly those with unique challenges such as ankylosing spondylitis, receive the best possible assessment and care for their bone health.
Subject of Research: Osteoporosis assessment using CT-based Hounsfield units in ankylosing spondylitis patients with bamboo spine.
Article Title: CT-based hounsfield unit as an alternative osteoporosis assessment in ankylosing spondylitis patients with bamboo spine.
Article References:
Hsiung, W., Lin, HH., Yao, YC. et al. CT-based hounsfield unit as an alternative osteoporosis assessment in ankylosing spondylitis patients with bamboo spine. Sci Rep 15, 35540 (2025). https://doi.org/10.1038/s41598-025-19528-z
Image Credits: AI Generated
DOI: 10.1038/s41598-025-19528-z
Keywords: Osteoporosis, Hounsfield units, Ankylosing spondylitis, Computed tomography, Bone mineral density, Bamboo spine, Diagnostic accuracy.
Tags: advancements in osteoporosis imaging technologyalternative assessment strategies for osteoporosisankylosing spondylitis and bone densitybamboo spine and osteoporosis riskbone mineral density measurement challengescomputed tomography for osteoporosis diagnosisCT Hounsfield units in osteoporosis assessmentlimitations of DXA in spinal disordersnon-invasive osteoporosis evaluation methodsnovel imaging techniques for osteoporosisosteoporosis public health concernsradiological features in ankylosing spondylitis.