In a groundbreaking revelation that could redefine our understanding of vascular diseases, researchers have uncovered a pivotal mechanism by which the enzyme KDM4B influences the calcification of vascular smooth muscle cells (VSMCs). This novel insight, recently detailed by Liu and colleagues in their 2025 publication in Cell Death Discovery, highlights the intricate interplay between epigenetic regulation and hormone signaling pathways in vascular pathology, potentially opening new avenues for targeted therapies in cardiovascular illnesses.
Vascular calcification, a pathological deposition of calcium phosphate crystals within blood vessel walls, dramatically increases cardiovascular morbidity and mortality. Despite its clinical importance, the molecular underpinnings driving this calcification process have remained enigmatic. The current study shines a spotlight on the enzyme KDM4B, a histone demethylase known for its role in modifying chromatin structure and gene expression, now implicated as a critical modulator of the estrogen receptor alpha (ERα) signaling axis in VSMCs.
Intriguingly, the estrogen receptor alpha (ERα) has been widely recognized for its cardioprotective effects, mediating diverse physiological processes through transcriptional control. What Liu et al. reveal is that KDM4B directly interacts with the ERα pathway to modulate the phenotypic switch of VSMCs from a contractile to an osteogenic state—a hallmark event precipitating vascular calcification. This discovery elucidates a significant epigenetic control layer governing hormonal influences within the vascular microenvironment.
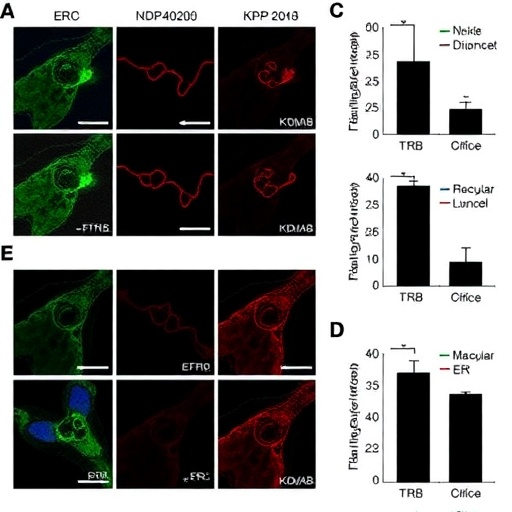
At the molecular level, the study delves into how KDM4B enzymatic activity removes methyl marks from histone proteins that repress ERα target genes. By demethylating Histone H3 Lysine 9 tri-methylation (H3K9me3) at specific gene loci, KDM4B enhances ERα-driven transcriptional programs that promote osteogenic differentiation in VSMCs. This finely tuned epigenetic remodeling facilitates the expression of bone-related genes, thereby hastening the pathologic calcification trajectory.
Functional assays demonstrating that knockdown or pharmacologic inhibition of KDM4B attenuates ERα-mediated osteogenic gene expression and decreases calcium deposition establish a compelling causal link. These findings suggest that KDM4B serves as a molecular switch integrating hormonal signals into epigenetic modifications, ultimately controlling VSMC fate decisions in the calcification process, a revelation with transformative potential in treating vascular stiffening and related diseases.
Further substantiating their mechanistic insights, the researchers utilized advanced genomic and proteomic techniques, including chromatin immunoprecipitation sequencing (ChIP-seq) and RNA sequencing (RNA-seq). These analyses delineated the comprehensive gene networks regulated by the KDM4B-ERα axis, uncovering previously unknown target genes implicated in osteogenic differentiation, inflammation, and extracellular matrix remodeling within the vascular milieu.
Importantly, the study also addresses the dynamic nature of ERα signaling, which can switch between protective and pathological roles depending on its epigenetic context. The involvement of KDM4B as an epigenetic ‘fine-tuner’ illustrates how hormone receptor signaling is intricately modulated beyond ligand binding, involving chromatin state changes that impact vascular cell phenotype and calcification outcomes.
This paradigm-shifting research not only deepens our comprehension of cardiovascular calcification but also underscores the therapeutic promise of targeting epigenetic enzymes like KDM4B. Since vascular calcification lacks effective direct treatments, interventions aimed at modulating KDM4B activity could pave the way for disease-modifying strategies that halt or reverse vessel stiffening and reduce cardiovascular risk.
As vascular calcification remains a major challenge in aging populations and those with metabolic disorders such as diabetes and chronic kidney disease, the implications of this study resonate widely. The link between an epigenetic enzyme and hormone receptor pathways opens interdisciplinary research frontiers, bridging molecular biology, cardiology, and endocrinology to innovate new treatments.
Moreover, by highlighting an epigenetic mechanism that interfaces with estrogen receptor signaling, this research may explain gender disparities observed in vascular disease prevalence and progression, providing a foundation for sex-specific therapeutic approaches. The nuanced understanding of how estrogen signaling is modulated could inform precision medicine initiatives targeting vascular calcification in women and men differently.
While these findings represent a monumental leap forward, further in vivo studies and clinical investigations will be essential to validate KDM4B as a bona fide therapeutic target. Additionally, exploring the regulatory networks upstream of KDM4B expression and activity could uncover even more intricate layers of control in vascular calcification pathogenesis.
Intriguingly, the discovery also prompts reconsideration of existing pharmacotherapies relating to estrogen signaling and histone demethylation inhibitors, prompting exploration into whether these agents might inadvertently modulate vascular calcification through affecting the KDM4B-ERα axis. Such considerations could influence clinical guidelines and inspire repurposing of known drugs.
Overall, this study redefines vascular calcification as a phenomenon governed not just by metabolic derangements but by epigenetic reprogramming orchestrated through hormone receptor pathways. The KDM4B-ERα nexus emerges as a master regulator dictating smooth muscle cell fate, and thereby vessel integrity, with broad implications for cardiovascular biology and treatment paradigms.
As the scientific community continues to unravel the complexities of vascular disease, the fresh insights offered by Liu et al. inject renewed optimism for conquering this pervasive health threat. The fusion of epigenetics and endocrinology illustrated here exemplifies the future of biomedical research, where integrated approaches illuminate hidden disease mechanisms and foster innovative therapeutics.
With mounting cardiovascular disease burden globally, translational advances leveraging this novel knowledge of KDM4B’s role could eventually translate into improved patient outcomes, extending lifespans and enhancing quality of life. Continued research inspired by these findings will doubtless catalyze breakthroughs in combating vascular calcification and its devastating consequences.
In conclusion, the elucidation of KDM4B as a critical modulator of ERα signaling in vascular smooth muscle cell calcification provides a groundbreaking molecular framework for understanding and potentially intervening in vascular calcification. This study marks a transformative advance in cardiovascular science, highlighting the power of epigenetic regulation in disease and paving the way toward next-generation, targeted therapies.
Subject of Research:
The molecular mechanisms underlying vascular smooth muscle cell calcification, focusing on the regulatory role of the histone demethylase KDM4B and its modulation of the estrogen receptor alpha (ERα) signaling pathway.
Article Title:
KDM4B modulates ERα signaling pathway to participate in vascular smooth muscle cell calcification.
Article References:
Liu, F., Lv, Y., Lin, Y. et al. KDM4B modulates ERα signaling pathway to participate in vascular smooth muscle cell calcification. Cell Death Discov. 11, 452 (2025). https://doi.org/10.1038/s41420-025-02765-6
Image Credits:
AI Generated
DOI:
https://doi.org/10.1038/s41420-025-02765-6
Tags: calcification of vascular smooth muscle cellscalcium phosphate crystal deposition in blood vesselscardiovascular morbidity and mortality factorsepigenetic regulation in cardiovascular diseasesERα signaling in vascular smooth muscle cellsestrogen receptor alpha cardioprotective effectshormone signaling pathways in vascular pathologyKDM4B enzyme in vascular calcificationmechanisms of vascular disease progressionphenotypic switch in vascular smooth muscle cellsrole of histone demethylase in gene expressiontargeted therapies for cardiovascular illnesses