In a medical case that has captured the attention of cardiologists and forensic pathologists alike, a recent autopsy revealed unexpected findings following the sudden perioperative death of an elderly female patient who had undergone aortic valve replacement surgery. This case highlights the complex interplay between surgical intervention and underlying cardiac pathology, underscoring the importance of meticulous preoperative assessment and the potential for silent yet fatal cardiac conditions, such as hypertrophic cardiomyopathy (HCM), even in elderly populations.
The patient, an elderly female, was admitted for aortic valve replacement (AVR), a common surgical procedure aimed at relieving the symptoms and risk associated with aortic valve diseases such as stenosis or insufficiency. Despite the advancements in surgical techniques and perioperative care, mortality risks remain, particularly in elderly patients with comorbidities. In this instance, the patient succumbed suddenly in the perioperative period, prompting a thorough forensic investigation to elucidate the cause of death.
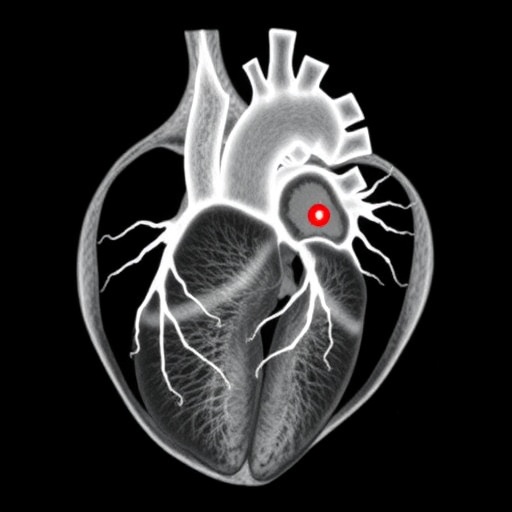
Autopsy findings revealed a striking diagnosis of hypertrophic cardiomyopathy, a genetic cardiac disorder characterized by abnormal thickening of the myocardial walls, most notably the interventricular septum. HCM is notoriously underdiagnosed, especially in elderly patients where its presentation can be atypical or masked by other cardiovascular diseases. The presence of HCM in this patient sheds light on the potential for this condition to contribute significantly to surgical risk and perioperative mortality.
Hypertrophic cardiomyopathy is a complex myocardial disorder, often inherited in an autosomal dominant pattern, involving mutations in genes encoding sarcomeric proteins. The resulting hypertrophy can cause obstruction of the left ventricular outflow tract, diastolic dysfunction, myocardial ischemia, and arrhythmias. These pathophysiological changes increase the risk of sudden cardiac death, particularly under physiological stress such as surgery, which may aggravate cardiac workload and provoke fatal arrhythmias.
This case illustrates the challenge in distinguishing hypertrophic cardiomyopathy in elderly patients, especially when it coexists with other cardiac conditions warranting surgical intervention. Traditionally considered a disease of the young, HCM’s relevance in older adults is gaining recognition due to increased life expectancy and improved diagnostic modalities. The autopsy’s role in confirming HCM in an unsuspected elderly patient is critical, serving as a cautionary tale for clinicians to maintain a high index of suspicion.
The perioperative period is a vulnerable window for patients with undiagnosed HCM. Hemodynamic fluctuations during anesthesia, surgical manipulation, and postoperative stress can precipitate adverse cardiac events such as left ventricular outflow obstruction exacerbation, malignant arrhythmias, and sudden cardiac death. This case starkly exemplifies how latent cardiac conditions can manifest catastrophically amidst the physiological upheaval of surgery.
Beyond the clinical implications, this case has legal and ethical dimensions. Sudden perioperative deaths often trigger medicolegal scrutiny, especially when unexpected findings emerge post-mortem. The identification of hypertrophic cardiomyopathy as the cause of death through autopsy provides essential closure for families and healthcare professionals, clarifying the etiology of death and potentially assuaging concerns about surgical negligence.
In addition to forensic significance, the findings reinforce the need for enhanced preoperative cardiac evaluation protocols, particularly for elderly patients scheduled for valve replacement surgeries. Non-invasive imaging modalities such as echocardiography and cardiac magnetic resonance imaging (MRI) can be instrumental in detecting myocardial hypertrophy and functional abnormalities indicative of HCM.
This case also raises pertinent questions about the integration of genetic screening and family history evaluation in pre-surgical workups. Given HCM’s heritable nature, the detection of this condition in an elderly patient invites consideration of familial screening to prevent catastrophic events in relatives who may harbor similar mutations but remain asymptomatic.
From a procedural standpoint, anesthetic and surgical teams must be cognizant of the risks posed by hypertrophic cardiomyopathy, particularly the propensity for dynamic left ventricular outflow tract obstruction and arrhythmogenesis. Tailoring perioperative management to mitigate these risks – such as optimizing fluid status, avoiding inotropic agents that exacerbate obstruction, and vigilant cardiac monitoring – is paramount.
Furthermore, this case underscores the critical role of comprehensive post-mortem examinations in advancing medical knowledge. Autopsy findings not only confirm clinical suspicions but also uncover occult conditions that may have significant prognostic and therapeutic implications. The documentation of HCM in an elderly patient after sudden perioperative death enriches the literature, guiding future clinical practice toward safer surgical outcomes.
The sudden nature of the perioperative death in the presence of underlying hypertrophic cardiomyopathy challenges the conventional risk stratification models that often prioritize valvular pathology over myocardial disease in elderly patients. This necessitates revisiting existing paradigms to incorporate more nuanced assessments capturing the full spectrum of cardiac risk factors.
Ultimately, this case report from Razak, Westaby, and Sheppard emphasizes a multilayered approach to cardiovascular surgery in the elderly: one that integrates detailed preoperative diagnostics, individualized perioperative care, and thorough post-mortem investigation. Such an approach promises to reduce unexpected deaths and improve overall patient safety in this vulnerable population.
The broader implications extend to cardiac surgery policies and guidelines, encouraging multidisciplinary collaboration between cardiologists, cardiac surgeons, anesthesiologists, and pathologists. Recognizing the silent yet deadly presence of hypertrophic cardiomyopathy is a step toward achieving these goals.
In conclusion, the sudden perioperative death of an elderly female following aortic valve replacement surgery, as highlighted in this case with autopsy findings of hypertrophic cardiomyopathy, serves as a powerful reminder of the hidden cardiac risks that may underlie ostensibly straightforward surgical cases. This case advocates for heightened clinical vigilance and comprehensive cardiac evaluation to safeguard patient lives in cardiovascular surgical practice.
Subject of Research: Sudden perioperative death related to hypertrophic cardiomyopathy in elderly patients undergoing aortic valve replacement surgery
Article Title: Sudden perioperative death post aortic valve replacement with autopsy showing hypertrophic cardiomyopathy in elderly female
Article References:
Razak, Z.A., Westaby, J. & Sheppard, M.N. Sudden perioperative death post aortic valve replacement with autopsy showing hypertrophic cardiomyopathy in elderly female. Int J Legal Med (2025). https://doi.org/10.1007/s00414-025-03544-9
Image Credits: AI Generated
Tags: advanced surgical techniques and risksaortic valve replacement complicationselderly population cardiac careforensic investigation in cardiac deathsgenetic factors in hypertrophic cardiomyopathyhypertrophic cardiomyopathy in elderly patientsmyocardial thickening and heart diseaseperioperative mortality riskspreoperative assessment for cardiac surgerysilent cardiac conditions in surgerysudden death after aortic valve replacementunexpected autopsy findings