In a groundbreaking advancement for neonatal respiratory care, researchers have unveiled a novel approach to optimizing positive end-expiratory pressure (PEEP) using electrical impedance tomography (EIT) in infants suffering from severe bronchopulmonary dysplasia (BPD). This pioneering study presents a feasible methodology to refine ventilator settings tailored specifically to the fragile and heterogeneous lung pathology characteristic of BPD, potentially transforming clinical management and patient outcomes in neonatal intensive care units (NICUs) worldwide.
Bronchopulmonary dysplasia remains a formidable challenge in neonatology, particularly affecting premature infants who require prolonged mechanical ventilation and oxygen therapy. Characterized by impaired alveolar development and chronic lung inflammation, severe BPD results in compromised respiratory function, making the delicate balance of ventilator support critical. Excessive PEEP can exacerbate lung injury, whereas inadequate PEEP leads to alveolar collapse and insufficient gas exchange. The determination of optimal PEEP, therefore, is paramount but notoriously difficult due to heterogeneous lung mechanics and regional ventilation abnormalities.
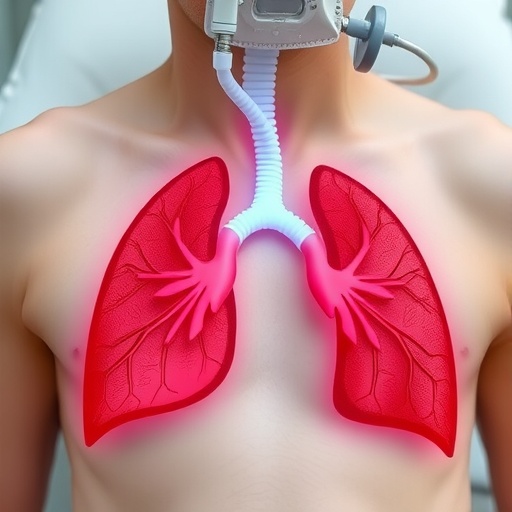
Electrical impedance tomography, a cutting-edge, non-invasive imaging modality, has emerged as a promising tool for bedside monitoring of lung ventilation distribution in real-time. By applying small alternating electrical currents through the chest and measuring resulting voltages, EIT produces cross-sectional images reflecting changes in lung impedance correlating with air content. This functional imaging enables clinicians to visualize regional ventilation, detect overdistension, and identify areas of collapse dynamically during mechanical ventilation. In this study, the researchers hypothesized that EIT-guided PEEP titration could pinpoint individualized optimal PEEP settings, mitigating lung injury risk and improving oxygenation.
The investigative team conducted meticulous EIT assessments in neonates diagnosed with severe BPD under mechanical ventilation. They systematically adjusted PEEP levels while continuously monitoring ventilation distribution patterns via EIT. This translational approach allowed them to identify PEEP values that maximized lung recruitment without causing overinflation, thereby defining an optimal ventilatory window unique to each infant’s pulmonary status. By leveraging EIT’s capacity to visualize real-time changes in regional ventilation, clinicians can precisely tailor ventilator parameters to the intricacies of each patient’s diseased lung architecture.
Importantly, the study illuminates how traditional methods of PEEP titration, often reliant on global measurements such as oxygen saturation or pulmonary compliance, can obscure critical regional heterogeneities in lung function typical of BPD. These conventional parameters risk underestimating areas prone to atelectasis or volutrauma. Conversely, EIT offers unparalleled spatial and temporal resolution, revealing ventilation inhomogeneities and guiding interventions that balance alveolar recruitment against overdistension, fundamentally enhancing ventilation strategies.
Technically, the feasibility of applying EIT in neonates with severe lung disease was a significant component of the study’s contribution. Neonatal PICUs face numerous challenges implanting new imaging technologies in vulnerable infants, including technical constraints related to thoracic size, electrode placement, and signal interpretation amidst heterogeneous lung tissue. The researchers overcame these hurdles, demonstrating adaptability of EIT systems in a highly fragile patient population while maintaining continuous, real-time ventilation monitoring with minimal clinical disruption.
The implications of this work extend beyond immediate ventilator management. Precise PEEP titration informed by EIT could reduce ventilator-induced lung injury—a primary driver of morbidity and prolonged hospitalization in infants with BPD. By avoiding both atelectrauma from underventilated regions and barotrauma from overdistended areas, this technique has the potential to decrease inflammatory cascades, promote lung healing, and ultimately improve long-term respiratory outcomes and quality of life.
Furthermore, integrating EIT into routine NICU protocols presents an opportunity to personalize neonatal respiratory therapy. Each infant’s lung disease in BPD is distinct, shaped by individual perinatal factors, inflammatory responses, and mechanical ventilation history. EIT-guided PEEP titration signifies a paradigm shift from static ventilator settings towards dynamic, personalized respiratory support, aligning with precision medicine principles in neonatology.
The study also draws attention to the broader utility of EIT as a bedside monitoring tool for other neonatal pulmonary conditions, such as respiratory distress syndrome, pulmonary hypertension, and congenital diaphragmatic hernia. Its non-invasive, radiation-free nature and capacity for continuous monitoring make it an ideal adjunct to existing diagnostics and therapeutic decision-making frameworks in fragile newborns.
Clinicians and respiratory therapists stand to benefit from enhanced training in interpreting EIT data, as the nuanced visualization of regional lung ventilation represents a new clinical skill set. Collaborative efforts between neonatologists, biomedical engineers, and nursing staff are essential to embed this technology effectively into clinical workflows, ensuring data is leveraged accurately to guide critical respiratory adjustments in real time.
Despite these promising results, the study underscores that EIT-guided PEEP titration requires further validation in larger, randomized controlled trials to assess impact on clinical outcomes such as duration of mechanical ventilation, incidence of chronic lung disease, and neurodevelopmental trajectories. Additionally, standardization of EIT electrode configurations, data processing algorithms, and interpretation criteria will be pivotal in streamlining its clinical adoption globally.
Nevertheless, this pioneering research marks a significant leap forward, positioning electrical impedance tomography at the forefront of neonatal respiratory medicine innovation. By enabling clinicians to visualize the lung’s invisible landscape and titrate PEEP with unprecedented precision, it opens new horizons for anesthetic safety, ventilator management, and neonatal care excellence.
In conclusion, the integration of EIT technology to guide PEEP titration in severe bronchopulmonary dysplasia represents an exciting convergence of bioengineering and neonatology. This approach promises to enhance the personalization and efficacy of ventilation strategies, lower the burden of lung injury, and improve survival and long-term health prospects of some of the most vulnerable patients—premature infants battling chronic lung disease.
As neonatal intensive care continues its rapid evolution fueled by technological innovation, the promise of electrical impedance tomography stands as a beacon for safer, smarter respiratory support. The successful demonstration of feasibility and clinical potential embodied in this study is a compelling call to further explore and harness this transformative technology, potentially rewriting respiratory care paradigms for the newborn intensive care landscape of tomorrow.
For families, clinicians, and healthcare systems dedicated to optimizing outcomes for infants with severe BPD, this research provides renewed hope that precision-guided ventilation may soon become standard practice—ushering in a new era where real-time lung imaging guides individualized care, safeguards delicate lungs, and ultimately changes the trajectory of neonatal respiratory disease for the better.
Subject of Research: Identifying optimal positive end-expiratory pressure with electrical impedance tomography guidance in severe bronchopulmonary dysplasia
Article Title: Identifying optimal positive end-expiratory pressure with electrical impedance tomography guidance in severe bronchopulmonary dysplasia
Article References:
Shui, J.E., LaVita, C.J., Alcala, G.C. et al. Identifying optimal positive end-expiratory pressure with electrical impedance tomography guidance in severe bronchopulmonary dysplasia. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02433-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41372-025-02433-8
Tags: challenges in neonatal mechanical ventilationchronic lung inflammation in premature babieselectrical impedance tomography in NICUsheterogeneous lung pathology in infantsimproving patient outcomes in severe BPDlung injury and PEEP balanceneonatal intensive care unit advancementsnon-invasive lung monitoring techniquesoptimizing PEEP in neonatal respiratory carereal-time lung ventilation imagingsevere bronchopulmonary dysplasia managementventilator settings for premature infants