A groundbreaking study from the Icahn School of Medicine at Mount Sinai has unveiled an unprecedentedly detailed map of brain cell interactions underlying Alzheimer’s disease, shedding new light on the molecular crosstalk that drives this devastating neurodegenerative condition. Published in the prestigious journal Cell on September 25, 2025, this research represents a major paradigm shift, moving beyond the classical hallmark proteins amyloid beta and tau, to unravel the complex protein networks mediating communication between neurons and glial cells. By leveraging advanced proteomic techniques, the investigators have identified crucial bio-molecular breakdowns that occur during disease progression, highlighting novel therapeutic targets with promising potential.
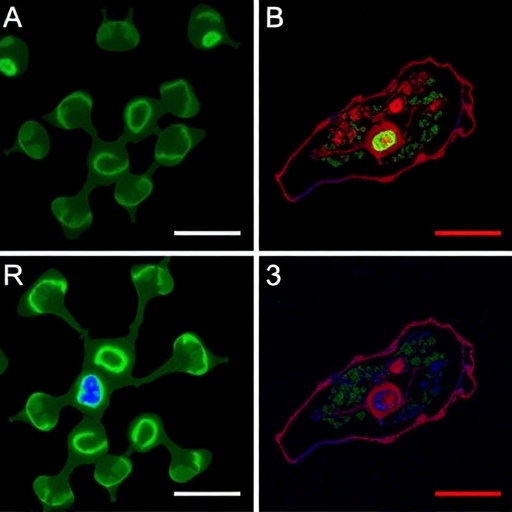
The study analyzed the proteomic landscape of brain tissue from nearly 200 individuals, encompassing both Alzheimer’s patients and healthy controls. Through an unbiased, unsupervised computational modeling approach, the team quantified expression levels and interactions across more than 12,000 proteins, generating comprehensive protein interaction networks. These networks revealed that the disruption of communication between neurons and the brain’s supporting glial cells—especially astrocytes and microglia—is a central event in the pathogenesis of Alzheimer’s disease. This breakdown in cellular crosstalk cultivates a neuroinflammatory milieu and fosters neural dysfunction, driving the progression of cognitive decline.
Traditionally, Alzheimer’s research has focused heavily on the accumulation of extracellular amyloid plaques and intracellular tau tangles as causative agents. However, the modest efficacy of many plaque-targeting therapies underscores that this pathological accumulation alone cannot fully account for disease mechanisms. The present study’s large-scale proteomic profiling, paired with sophisticated network modeling, moves beyond these limitations by capturing the dynamic interplay of thousands of proteins within complex brain ecosystems, enabling the identification of entire dysregulated molecular systems rather than isolated pathogenic molecules.
Central to the study’s findings was the identification of key “driver” proteins that orchestrate maladaptive signaling cascades in Alzheimer’s disease. Among these, the protein AHNAK emerged as a standout candidate. AHNAK is predominantly expressed in astrocytes, a class of glial cells critical for neuronal support and homeostasis. The researchers demonstrated that AHNAK expression escalates in correlation with disease severity and aligns with increased levels of toxic amyloid beta and tau proteins. Intriguingly, experimental reduction of AHNAK in human stem cell-derived brain cell cultures attenuated tau pathology and restored neuronal function, suggesting that modulating AHNAK activity could form the basis for a novel therapeutic strategy.
The implications of targeting AHNAK are profound. Astrocytes have traditionally been viewed as passive support cells, but mounting evidence now places them as active regulators of neuronal health and inflammation. AHNAK’s role in mediating astrocyte-neuron communication places it at the nexus of processes controlling neuronal viability, synaptic integrity, and inflammatory response. By dampening AHNAK-driven pathological signaling, it may be possible to halt or even reverse the damaging cascade that leads to neurodegeneration.
Moreover, the research uncovered over 300 additional proteins involved in Alzheimer’s pathophysiology, many of which have been rarely studied in this context. This vast catalog of protein alterations broadens the horizon for future investigations and drug discovery. The findings also underscore the complex heterogeneity of Alzheimer’s disease—demonstrating that factors such as gender and genetic background, including carriage of the APOE4 allele (the strongest known genetic risk factor for late-onset Alzheimer’s), significantly influence the proteomic network configurations and, consequently, disease progression patterns.
The use of advanced computational modeling approaches was instrumental in discerning these intricate protein interaction networks from the enormous data sets generated by quantitative proteomics. These algorithms constructed multilevel maps of cellular communication pathways, pinpointing molecular hubs and disruptions, thus enabling the recognition of system-level breakdowns rather than isolated protein changes. Such integrative systems biology approaches herald a new era in understanding complex brain disorders like Alzheimer’s.
Co-senior author Bin Zhang, PhD, emphasized that this study represents a shift in conceptualizing Alzheimer’s disease—from a pathological accumulation of protein tangles to a failure of the entire brain ecosystem’s communication networks. The pathological hyperactivation of glial cells coupled with declining neuronal functionality and elevated inflammation suggests an asynchronous dialogue among brain cells that must be restored to maintain cognitive health.
Furthermore, the publicly accessible data repository from this research expedites collective scientific progress, allowing researchers worldwide to delve into these proteomic networks and test hypotheses experimentally, accelerating the quest for effective Alzheimer’s treatments. This open science approach exemplifies the future of biomedical research, wherein collaborative data sharing is key to solving complex diseases.
In essence, this study’s insights offer a compelling framework for developing multifaceted therapeutic approaches that restore cellular communication and homeostasis. Rather than singularly targeting amyloid or tau, interventions aimed at rebalancing glia-neuron interactions and mitigating neuroinflammation hold the promise of more effective disease modification.
Researchers and clinicians alike are hopeful that this comprehensive proteomic modeling will lead to breakthroughs in understanding and treating Alzheimer’s. By revealing the molecular symphony of brain cells disrupted during the disease, these findings usher in a new era where “cellular conversations” become the focus of innovative interventions, potentially transforming outcomes for millions facing Alzheimer’s worldwide.
Subject of Research: Human tissue samples
Article Title: Multiscale Proteomic Modeling Reveals Interacting Neuronal and Glial Protein Networks Driving Alzheimer’s Disease Pathogenesis
News Publication Date: 25-Sep-2025
Web References: https://doi.org/10.1016/j.cell.2025.08.038
References: NIH grant numbers U01AG046170, RF1AG054014, RF1AG057440, R01AG057907, and others as specified
Keywords: Neurodegenerative diseases
Tags: advanced computational modeling in biologyAlzheimer’s disease mechanismsbrain cell communicationbreakthrough Alzheimer’s research findingsglial cell interactions in brain healthmolecular crosstalk in neuronsneurodegenerative conditionsneuroinflammation and cognitive declineprotein interaction mapproteomic landscape analysisproteomic techniques in neurosciencetherapeutic targets for Alzheimer’s